Polymers for Surgery Implants
Seyyed Mojtaba Mousavi, Masoomeh Yari Kalashgrani, Nadiar M. Mussin, Amin Tamadon, Chin Wei Lai
Polymer surgery implants have emerged as a revolutionary advancement in the field of medical technology, offering innovative solutions for various surgical procedures. These implants are crafted from biocompatible and biodegradable polymers, meticulously engineered to mimic the properties of human tissues. Their unique composition allows for seamless integration into the body, minimizing the risk of rejection and promoting natural healing processes. Polymer implants have found widespread applications in orthopedics, reconstructive surgery, and tissue engineering. They serve as scaffolds for tissue regeneration, providing structural support and facilitating the growth of new cells and blood vessels. Additionally, these implants can be designed to release therapeutic agents, such as antibiotics or growth factors, directly at the implantation site, enhancing the healing process and reducing the risk of infections. The versatility of polymer implants extends beyond their structural and therapeutic capabilities. They can be tailored to specific patient needs, with customizable shapes, sizes, and degradation rates. This personalized approach ensures optimal outcomes and improved patient comfort. As research continues to advance, polymer implants hold immense potential for transforming surgical practices, offering safer, more effective, and patient-centric solutions.
Keywords
Polymer, Surgery Implant, Biodegradable Polymers, Natural and Synthetic Polymeric
Published online 2/15/2025, 22 pages
Citation: Seyyed Mojtaba Mousavi, Masoomeh Yari Kalashgrani, Nadiar M. Mussin, Amin Tamadon, Chin Wei Lai, Polymers for Surgery Implants, Materials Research Foundations, Vol. 172, pp 65-86, 2025
DOI: https://doi.org/10.21741/9781644903353-3
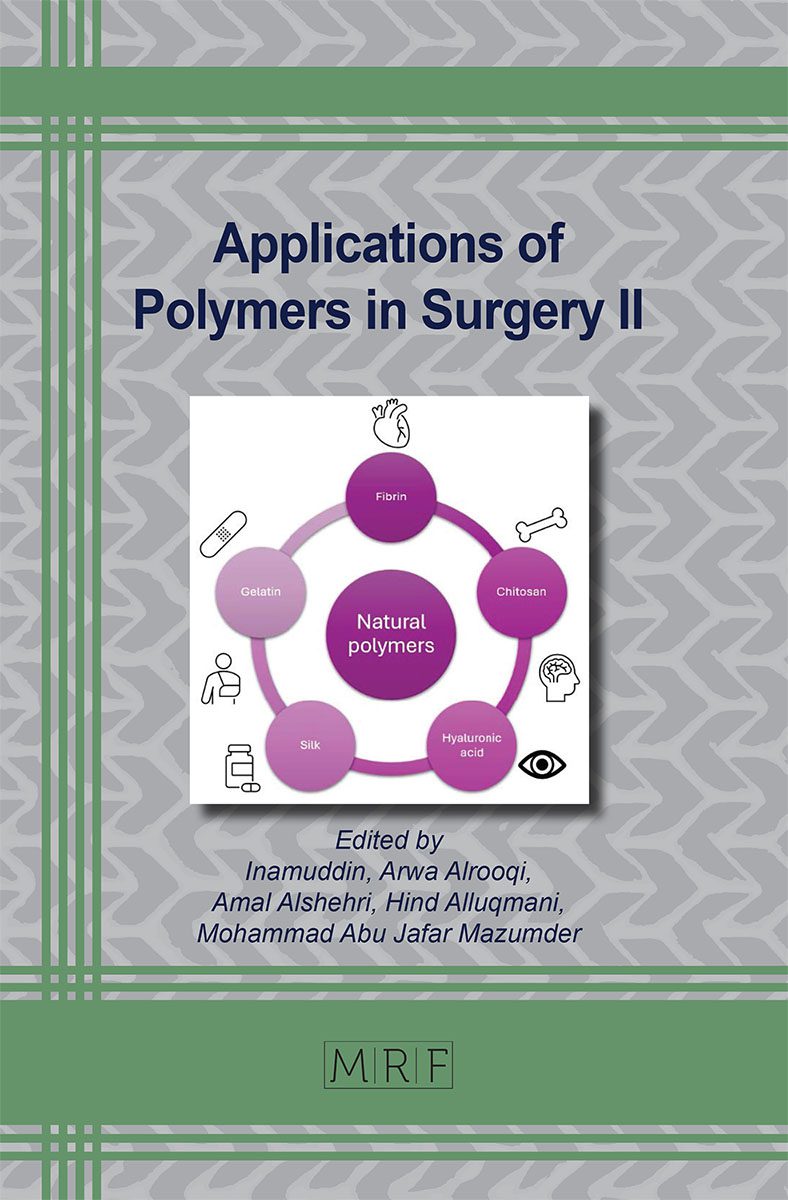
Part of the book on Applications of Polymers in Surgery II
References
[1] Seok, S., Polymer-based biocompatible packaging for implantable devices: packaging method, materials, and reliability simulation. Micromachines, 2021. 12(9): p. 1020. https://doi.org/10.3390/mi12091020
[2] Darie-Niță, R.N., M. Râpă, and S. Frąckowiak, Special features of polyester-based materials for medical applications. Polymers, 2022. 14(5): p. 951. https://doi.org/10.3390/polym14050951
[3] Men, L., et al., Biocompatible polymers with tunable mechanical properties and conductive functionality on two-photon 3D printing. RSC advances, 2023. 13(13): p. 8586-8593. https://doi.org/10.1039/D2RA07464H
[4] Arefin, A.M., et al., Polymer 3D printing review: Materials, process, and design strategies for medical applications. Polymers, 2021. 13(9): p. 1499. https://doi.org/10.3390/polym13091499
[5] Pires, P.C., et al., Polymer-based biomaterials for pharmaceutical and biomedical applications: A focus on topical drug administration. European Polymer Journal, 2023. 187: p. 111868. https://doi.org/10.1016/j.eurpolymj.2023.111868
[6] Khan, W., et al., Implantable medical devices. Focal controlled drug delivery, 2014: p. 33-59. https://doi.org/10.1007/978-1-4614-9434-8_2
[7] Lin, S., L. Kimble, and D. Bhattacharyya, Polymer blends and composites for biomedical applications. Biomaterials for Implants and Scaffolds, 2017: p. 195-235. https://doi.org/10.1007/978-3-662-53574-5_7
[8] Suzuki, S. and Y. Ikada, Medical applications. Poly (Lactic Acid) Synthesis, Structures, Properties, Processing, Applications, and End of Life, 2022: p. 581-604. https://doi.org/10.1002/9781119767480.ch25
[9] Kirillova, A., et al., Fabrication of biomedical scaffolds using biodegradable polymers. Chemical reviews, 2021. 121(18): p. 11238-11304. https://doi.org/10.1021/acs.chemrev.0c01200
[10] Jayarama Reddy, V., et al., Nanofibrous structured biomimetic strategies for skin tissue regeneration. Wound Repair and regeneration, 2013. 21(1): p. 1-16. https://doi.org/10.1111/j.1524-475X.2012.00861.x
[11] Ravichandran, R., et al., Expression of cardiac proteins in neonatal cardiomyocytes on PGS/fibrinogen core/shell substrate for Cardiac tissue engineering. International journal of cardiology, 2013. 167(4): p. 1461-1468. https://doi.org/10.1016/j.ijcard.2012.04.045
[12] Gandhimathi, C., et al., Mimicking nanofibrous hybrid bone substitute for mesenchymal stem cells differentiation into osteogenesis. Macromolecular bioscience, 2013. 13(6): p. 696-706. https://doi.org/10.1002/mabi.201200435
[13] Naveena, N., et al., Biomimetic composites and stem cells interaction for bone and cartilage tissue regeneration. Journal of Materials Chemistry, 2012. 22(12): p. 5239-5253. https://doi.org/10.1039/c1jm14401d
[14] Nair, L.S. and C.T. Laurencin, Biodegradable polymers as biomaterials. Progress in polymer science, 2007. 32(8-9): p. 762-798. https://doi.org/10.1016/j.progpolymsci.2007.05.017
[15] Sarem, M., F. Moztarzadeh, and M. Mozafari, How can genipin assist gelatin/carbohydrate chitosan scaffolds to act as replacements of load-bearing soft tissues? Carbohydrate polymers, 2013. 93(2): p. 635-643. https://doi.org/10.1016/j.carbpol.2012.11.099
[16] Yazdanpanah, A., et al., Synthesis and Characterization of Polylactic Acid Tubular Scaffolds with Improved Mechanical Properties for Vascular Tissue Engineering. Trends in Biomaterials & Artificial Organs, 2014. 28(3).
[17] Zarrintaj, P., et al., A facile route to the synthesis of anilinic electroactive colloidal hydrogels for neural tissue engineering applications. Journal of colloid and interface science, 2018. 516: p. 57-66. https://doi.org/10.1016/j.jcis.2018.01.044
[18] Gholipourmalekabadi, M., et al., Silk fibroin/amniotic membrane 3D bi-layered artificial skin. Biomedical Materials, 2018. 13(3): p. 035003. https://doi.org/10.1088/1748-605X/aa999b
[19] Ranella, A., et al., Tuning cell adhesion by controlling the roughness and wettability of 3D micro/nano silicon structures. Acta biomaterialia, 2010. 6(7): p. 2711-2720. https://doi.org/10.1016/j.actbio.2010.01.016
[20] Hoefling, M., et al., Interaction of amino acids with the Au (111) surface: adsorption free energies from molecular dynamics simulations. Langmuir, 2010. 26(11): p. 8347-8351. https://doi.org/10.1021/la904765u
[21] Meder, F., et al., Protein adsorption on colloidal alumina particles functionalized with amino, carboxyl, sulfonate and phosphate groups. Acta biomaterialia, 2012. 8(3): p. 1221-1229. https://doi.org/10.1016/j.actbio.2011.09.014
[22] Rahmati, M., et al., Biomaterials for regenerative medicine: Historical perspectives and current trends. Cell Biology and Translational Medicine, Volume 4: Stem Cells and Cell Based Strategies in Regeneration, 2018: p. 1-19. https://doi.org/10.1007/5584_2018_278
[23] Cleland, J.L., A. Daugherty, and R. Mrsny, Emerging protein delivery methods. Current opinion in biotechnology, 2001. 12(2): p. 212-219. https://doi.org/10.1016/S0958-1669(00)00202-0
[24] Morishita, M. and N.A. Peppas, Is the oral route possible for peptide and protein drug delivery? Drug discovery today, 2006. 11(19-20): p. 905-910. https://doi.org/10.1016/j.drudis.2006.08.005
[25] Sofini, P., et al., Biomedical Applications of Natural and Synthetic Polymer based Nanocomposites. Journal of Biomaterials science. Polymer Edition, 2023: p. 1-44.
[26] Satchanska, G., S. Davidova, and P.D. Petrov, Natural and Synthetic Polymers for Biomedical and Environmental Applications. Polymers, 2024. 16(8): p. 1159. https://doi.org/10.3390/polym16081159
[27] Chahal, S., A. Kumar, and F.S.J. Hussian, Development of biomimetic electrospun polymeric biomaterials for bone tissue engineering. A review. Journal of biomaterials science, polymer edition, 2019. 30(14): p. 1308-1355. https://doi.org/10.1080/09205063.2019.1630699
[28] Rodríguez, G.R., T. Patrício, and J.D. López, Natural polymers for bone repair, in Bone Repair Biomaterials. 2019, Elsevier. p. 199-232. https://doi.org/10.1016/B978-0-08-102451-5.00008-1
[29] Hacker, M.C., J. Krieghoff, and A.G. Mikos, Synthetic polymers, in Principles of regenerative medicine. 2019, Elsevier. p. 559-590. https://doi.org/10.1016/B978-0-12-809880-6.00033-3
[30] Al-Shalawi, F.D., et al., Biodegradable synthetic polymer in orthopaedic application: A review. Materials Today: Proceedings, 2023. 74: p. 540-546. https://doi.org/10.1016/j.matpr.2022.12.254
[31] Budak, K., O. Sogut, and U. Aydemir Sezer, A review on synthesis and biomedical applications of polyglycolic acid. Journal of polymer research, 2020. 27: p. 1-19. https://doi.org/10.1007/s10965-020-02187-1
[32] Simionescu, B.C. and D. Ivanov, Natural and synthetic polymers for designing composite materials, in Handbook of bioceramics and biocomposites. 2016, Springer. p. 233-286. https://doi.org/10.1007/978-3-319-12460-5_11
[33] Prete, S., et al., Natural and synthetic polymeric biomaterials for application in wound management. Journal of Functional Biomaterials, 2023. 14(9): p. 455. https://doi.org/10.3390/jfb14090455
[34] Damodaran, V.B., D. Bhatnagar, and N.S. Murthy, Biomedical polymers: Synthesis and processing. 2016: Springer. https://doi.org/10.1007/978-3-319-32053-3
[35] Venkatraman, S., F. Boey, and L.L. Lao, Implanted cardiovascular polymers: Natural, synthetic and bio-inspired. Progress in Polymer Science, 2008. 33(9): p. 853-874. https://doi.org/10.1016/j.progpolymsci.2008.07.001
[36] Donnaloja, F., et al., Natural and synthetic polymers for bone scaffolds optimization. Polymers, 2020. 12(4): p. 905. https://doi.org/10.3390/polym12040905
[37] Claes, L. and A. Ignatius, Development of new, biodegradable implants. Der chirurg, 2002. 73: p. 990-996. https://doi.org/10.1007/s00104-002-0543-0
[38] Tian, W., et al., The influence of advancing age on implantation of drug‐eluting stents. Catheterization and Cardiovascular Interventions, 2016. 88(4): p. 516-521. https://doi.org/10.1002/ccd.26333
[39] Kumar, A. and J. Pillai, Implantable drug delivery systems: An overview. Nanostructures for the engineering of cells, tissues and organs, 2018: p. 473-511. https://doi.org/10.1016/B978-0-12-813665-2.00013-2
[40] Ranjan, N., Chitosan with PVC polymer for biomedical applications: A bibliometric analysis. Materials Today: Proceedings, 2023. 81: p. 894-898. https://doi.org/10.1016/j.matpr.2021.04.274
[41] Saadati, A., M. Hasanzadeh, and F. Seidi, Biomedical application of hyperbranched polymers: Recent Advances and challenges. TrAC Trends in Analytical Chemistry, 2021. 142: p. 116308. https://doi.org/10.1016/j.trac.2021.116308
[42] Li, L., et al., Reservoir-Style Polymeric Drug Delivery Systems: Empirical and Predictive Models for Implant Design. Pharmaceuticals, 2022. 15(10): p. 1226. https://doi.org/10.3390/ph15101226
[43] Steinbüchel, A., Non-biodegradable biopolymers from renewable resources: perspectives and impacts. Current opinion in biotechnology, 2005. 16(6): p. 607-613. https://doi.org/10.1016/j.copbio.2005.10.011
[44] Lin, Q., Synthetic Non-Biodegradable Polymers, in Introduction to Biomaterials. 2006, World Scientific. p. 172-186. https://doi.org/10.1142/9789812700858_0011
[45] Martínez-Rus, F., et al., Fracture resistance of crowns cemented on titanium and zirconia implant abutments: a comparison of monolithic versus manually veneered all-ceramic systems. International Journal of Oral & Maxillofacial Implants, 2012. 27(6).
[46] Amini-Fazl, M.S., Biodegradation study of PLGA as an injectable in situ depot-forming implant for controlled release of paclitaxel. Polymer Bulletin, 2021: p. 1-14. https://doi.org/10.1007/s00289-020-03347-5
[47] Sun, L., et al., Advances in physiologically relevant actuation of shape memory polymers for biomedical applications. Polymer Reviews, 2021. 61(2): p. 280-318. https://doi.org/10.1080/15583724.2020.1825487
[48] de Romero, B.C., et al., Oral post-surgical healing with polyglycolic acid suture. Open Access Research Journal of Biology and Pharmacy, 2022. 5(2): p. 082-087. https://doi.org/10.53022/oarjbp.2022.5.2.0056
[49] Arun, Y., R. Ghosh, and A.J. Domb, Poly (ester-anhydrides) Derived from Esters of Hydroxy Acid and Cyclic Anhydrides. Biomacromolecules, 2022. 23(8): p. 3417-3428. https://doi.org/10.1021/acs.biomac.2c00542
[50] Kuznetsova, D., et al., Scaffold-and cell system-based bone grafts in tissue engineering. Medical Technologies in Medicine/Sovremennye Tehnologii v Medicine, 2014. 6(4).
[51] Guarino, V., F. Causa, and L. Ambrosio, Porosity and mechanical properties relationship in PCL porous scaffolds. Journal of Applied Biomaterials and Biomechanics, 2007. 5(3): p. 149-157.
[52] Mobaraki, M., et al., Bioinks and bioprinting: A focused review. Bioprinting, 2020. 18: p. e00080. https://doi.org/10.1016/j.bprint.2020.e00080
[53] Mora-Boza, A., et al., Glycerylphytate as an ionic crosslinker for 3D printing of multi-layered scaffolds with improved shape fidelity and biological features. Biomaterials science, 2020. 8(1): p. 506-516. https://doi.org/10.1039/C9BM01271K
[54] Ornaghi Jr, H.L., F.M. Monticeli, and L.D. Agnol, A Review on Polymers for Biomedical Applications on Hard and Soft Tissues and Prosthetic Limbs. Polymers, 2023. 15(19): p. 4034. https://doi.org/10.3390/polym15194034
[55] Al-Shalawi, F.D., et al., Biomaterials as implants in the orthopedic field for regenerative medicine: metal versus synthetic polymers. Polymers, 2023. 15(12): p. 2601. https://doi.org/10.3390/polym15122601
[56] Kovylin, R., D.Y. Aleynik, and I. Fedushkin, Modern porous polymer implants: synthesis, properties, and application. Polymer Science, Series C, 2021. 63: p. 29-46. https://doi.org/10.1134/S1811238221010033
[57] Ogay, V., et al., Progress and prospects of polymer-based drug delivery systems for bone tissue regeneration. Polymers, 2020. 12(12): p. 2881. https://doi.org/10.3390/polym12122881
[58 Kuang, T., et al., A facile approach to fabricate load-bearing porous polymer scaffolds for bone tissue engineering. Advanced Composites and Hybrid Materials, 2022. 5(2): p. 1376-1384. https://doi.org/10.1007/s42114-022-00418-1
[59] Xu, L., et al., Bioactive pore‐forming bone adhesives facilitating cell ingrowth for fracture healing. Advanced Materials, 2020. 32(10): p. 1907491. https://doi.org/10.1002/adma.201907491
[60] Li, X., et al., Development of functionally graded porous titanium/silk fibroin composite scaffold for bone repair. Materials Letters, 2021. 282: p. 128670. https://doi.org/10.1016/j.matlet.2020.128670
[61] Battiston, K., et al., Polymer-free corticosteroid dimer implants for controlled and sustained drug delivery. Nature Communications, 2021. 12(1): p. 2875. https://doi.org/10.1038/s41467-021-23232-7
[62] Teo, A.J., et al., Polymeric biomaterials for medical implants and devices. ACS Biomaterials Science & Engineering, 2016. 2(4): p. 454-472. https://doi.org/10.1021/acsbiomaterials.5b00429
[63] Seal, C., K. Vince, and M. Hodgson. Biodegradable surgical implants based on magnesium alloys-A review of current research. in IOP conference series: materials science and engineering. 2009. IOP Publishing. https://doi.org/10.1088/1757-899X/4/1/012011
[64] Sumner, D., Long-term implant fixation and stress-shielding in total hip replacement. Journal of Biomechanics, 2015. 48(5): p. 797-800. https://doi.org/10.1016/j.jbiomech.2014.12.021
[65] On, S.-W., et al., Bioabsorbable osteofixation materials for maxillofacial bone surgery: A review on polymers and magnesium-based materials. Biomedicines, 2020. 8(9): p. 300. https://doi.org/10.3390/biomedicines8090300
[66] Giannoudis, P.V., T.A. Einhorn, and D. Marsh, Fracture healing: the diamond concept. injury, 2007. 38: p. S3-S6. https://doi.org/10.1016/S0020-1383(08)70003-2
[67] Andrzejowski, P. and P.V. Giannoudis, The ‘diamond concept’for long bone non-union management. Journal of Orthopaedics and Traumatology, 2019. 20: p. 1-13. https://doi.org/10.1186/s10195-019-0528-0
[68] Clark, D., et al., Effects of aging on fracture healing. Current osteoporosis reports, 2017. 15: p. 601-608. https://doi.org/10.1007/s11914-017-0413-9
[69] Jin, W. and P.K. Chu, Orthopedic implants. Encyclopedia of biomedical engineering, 2019. 1(3): p. 425-439. https://doi.org/10.1016/B978-0-12-801238-3.10999-7
[70] Wang, J.L., et al., Biodegradable magnesium‐based implants in orthopedics-a general review and perspectives. Advanced science, 2020. 7(8): p. 1902443. https://doi.org/10.1002/advs.201902443
[71] Jia, L., et al., Polydopamine-assisted surface modification for orthopaedic implants. Journal of orthopaedic translation, 2019. 17: p. 82-95. https://doi.org/10.1016/j.jot.2019.04.001
[72] Huang, B., et al., Absorbable implants in sport medicine and arthroscopic surgery: A narrative review of recent development. Bioactive Materials, 2024. 31: p. 272-283. https://doi.org/10.1016/j.bioactmat.2023.08.015
[73] Wong, W.-K., et al., Polymer-Metal Composite Healthcare Materials: From Nano to Device Scale. Journal of Composites Science, 2022. 6(8): p. 218. https://doi.org/10.3390/jcs6080218
[74] Durham III, J.W., et al., Hydroxyapatite coating on PEEK implants: Biomechanical and histological study in a rabbit model. Materials Science and Engineering: C, 2016. 68: p. 723-731. https://doi.org/10.1016/j.msec.2016.06.049
[75] Wei, Y., et al., Study of polymethylmethacrylate/tricalcium silicate composite cement for orthopedic application. biomedical journal, 2023. 46(3): p. 100540. https://doi.org/10.1016/j.bj.2022.05.005
[76] Ghasemi, F., et al., Different modification methods of poly methyl methacrylate (PMMA) bone cement for orthopedic surgery applications. Archives of Bone and Joint Surgery, 2023. 11(8): p. 485.
[77] Zheng, Z., et al., Strategies to improve bioactive and antibacterial properties of polyetheretherketone (PEEK) for use as orthopedic implants. Materials Today Bio, 2022. 16: p. 100402. https://doi.org/10.1016/j.mtbio.2022.100402
[78] Molinar-Díaz, J., et al., Poly-Ether-Ether-Ketone (PEEK) Biomaterials and Composites: Challenges, Progress, and Opportunities. Polymer Reviews, 2024: p. 1-39. https://doi.org/10.1080/15583724.2024.2406965
[79] Said, A., Ultra-High-Molecular-Weight-Polyethylene (UHMWPE) as Desired Polymer Material for Biomedical. Khalij-Libya Journal of Dental and Medical Research, 2022: p. 11-16. https://doi.org/10.47705/kjdmr.216103
[80] Cui, M., et al., Developments of polyurethane in biomedical applications: A review. Resources Chemicals and Materials, 2023. https://doi.org/10.1016/j.recm.2023.07.004
[81] Sternberg, K., Current requirements for polymeric biomaterials in otolaryngology. GMS current topics in otorhinolaryngology, head and neck surgery, 2009. 8.
[82] Tan, F., et al., Recent advances in the implant-based drug delivery in otorhinolaryngology. Acta Biomaterialia, 2020. 108: p. 46-55. https://doi.org/10.1016/j.actbio.2020.04.012
[83] Rippy, M.K., et al., Evaluation of absorbable PLA nasal implants in an ovine model. Laryngoscope Investigative Otolaryngology, 2018. 3(3): p. 156-161. https://doi.org/10.1002/lio2.166
[84] Lehner, E., et al., Intracochlear PLGA based implants for dexamethasone release: challenges and solutions. International Journal of Pharmaceutics: X, 2019. 1: p. 100015. https://doi.org/10.1016/j.ijpx.2019.100015
[85] Plontke, S.K., et al., Controlled release dexamethasone implants in the round window niche for salvage treatment of idiopathic sudden sensorineural hearing loss. Otology & Neurotology, 2014. 35(7): p. 1168-1171. https://doi.org/10.1097/MAO.0000000000000434
[86] Spałek, J., et al., Biocompatible materials in otorhinolaryngology and their antibacterial properties. International Journal of Molecular Sciences, 2022. 23(5): p. 2575. https://doi.org/10.3390/ijms23052575
[87] Fredenberg, S., et al., The mechanisms of drug release in poly (lactic-co-glycolic acid)-based drug delivery systems-A review. International journal of pharmaceutics, 2011. 415(1-2): p. 34-52. https://doi.org/10.1016/j.ijpharm.2011.05.049
[88] Bode, C., et al., In-situ forming PLGA implants for intraocular dexamethasone delivery. International journal of pharmaceutics, 2018. 548(1): p. 337-348. https://doi.org/10.1016/j.ijpharm.2018.07.013
[89] Kim, H.M. and S.J. Woo, Ocular drug delivery to the retina: current innovations and future perspectives. Pharmaceutics, 2021. 13(1): p. 108. https://doi.org/10.3390/pharmaceutics13010108
[90] Bourges, J., et al., Intraocular implants for extended drug delivery: therapeutic applications. Advanced drug delivery reviews, 2006. 58(11): p. 1182-1202. https://doi.org/10.1016/j.addr.2006.07.026
[91] Lynch, C., et al., Advances in biodegradable nano-sized polymer-based ocular drug delivery. Polymers, 2019. 11(8): p. 1371. https://doi.org/10.3390/polym11081371
[92] Gupta, B., et al., Cellulosic polymers for enhancing drug bioavailability in ocular drug delivery systems. Pharmaceuticals, 2021. 14(11): p. 1201. https://doi.org/10.3390/ph14111201
[93] Mahlumba, P., et al., Stimuli-responsive polymeric systems for controlled protein and peptide delivery: future implications for ocular delivery. Molecules, 2016. 21(8): p. 1002. https://doi.org/10.3390/molecules21081002
[94] Witika, B.A., et al., Nano co-crystal embedded stimuli-responsive hydrogels: A potential approach to treat HIV/AIDS. Pharmaceutics, 2021. 13(2): p. 127. https://doi.org/10.3390/pharmaceutics13020127
[95] Medeiros, F.A., et al., Phase 3, randomized, 20-month study of bimatoprost implant in open-angle glaucoma and ocular hypertension (ARTEMIS 1). Ophthalmology, 2020. 127(12): p. 1627-1641. https://doi.org/10.1016/j.ophtha.2020.06.018
[96] Allyn, M.M., et al., Considerations for polymers used in ocular drug delivery. Frontiers in Medicine, 2022. 8: p. 787644. https://doi.org/10.3389/fmed.2021.787644
[97] Duraccio, D., F. Mussano, and M.G. Faga, Biomaterials for dental implants: current and future trends. Journal of Materials Science, 2015. 50: p. 4779-4812. https://doi.org/10.1007/s10853-015-9056-3
[98] Liu, X., P.K. Chu, and C. Ding, Surface modification of titanium, titanium alloys, and related materials for biomedical applications. Materials Science and Engineering: R: Reports, 2004. 47(3-4): p. 49-121. https://doi.org/10.1016/j.mser.2004.11.001
[99] Dhatrak, P., et al., Influence of cutting flutes on stress distribution for selected dental implants: numerical studies. Materials Today: Proceedings, 2021. 38: p. 2680-2686. https://doi.org/10.1016/j.matpr.2020.08.476
[100] Samieirad, S., et al., Tapered versus cylindrical implant: Which shape inflicts less pain after dental implant surgery? A clinical trial. Journal of Oral and Maxillofacial Surgery, 2019. 77(7): p. 1381-1388. https://doi.org/10.1016/j.joms.2019.02.027
[101] Fang, K., et al., Immobilization of chitosan film containing semaphorin 3A onto a microarc oxidized titanium implant surface via silane reaction to improve MG63 osteogenic differentiation. International Journal of Nanomedicine, 2014: p. 4649-4657. https://doi.org/10.2147/IJN.S68895