Polymers for the Production of Conventional Dosage Forms
Maria Lúcia Mendonça Costa, Layla Ribeiro Lucena, Brenda Maria Silva Bezerra, João Augusto Oshiro-Júnior, Bruna Galdorfini Chiari-Andréo
Performing a surgical procedure aims to improve the patient’s health and quality of life. Despite several controls and the advances experienced in this area, there is invariably aggression in organs and tissues in these procedures, subsequently requiring their repair. For this purpose, there are pharmacological resources to guarantee good results, prevent infections, control pain, contribute to the psychological care of patients, and improve the quality of healing. Pharmaceutical dosage forms can carry molecules of interest and contribute to the repair process. In these dosage forms various polymers can be used. Therefore, this chapter discusses the classifications of these different polymers, their particularities, and their use in medicines.
Keywords
Polymers, Pharmaceutical Dosage Forms, Excipients, Drug Delivery Systems
Published online 2/15/2025, 17 pages
Citation: Maria Lúcia Mendonça Costa, Layla Ribeiro Lucena, Brenda Maria Silva Bezerra, João Augusto Oshiro-Júnior, Bruna Galdorfini Chiari-Andréo, Polymers for the Production of Conventional Dosage Forms, Materials Research Foundations, Vol. 172, pp 246-262, 2025
DOI: https://doi.org/10.21741/9781644903353-10
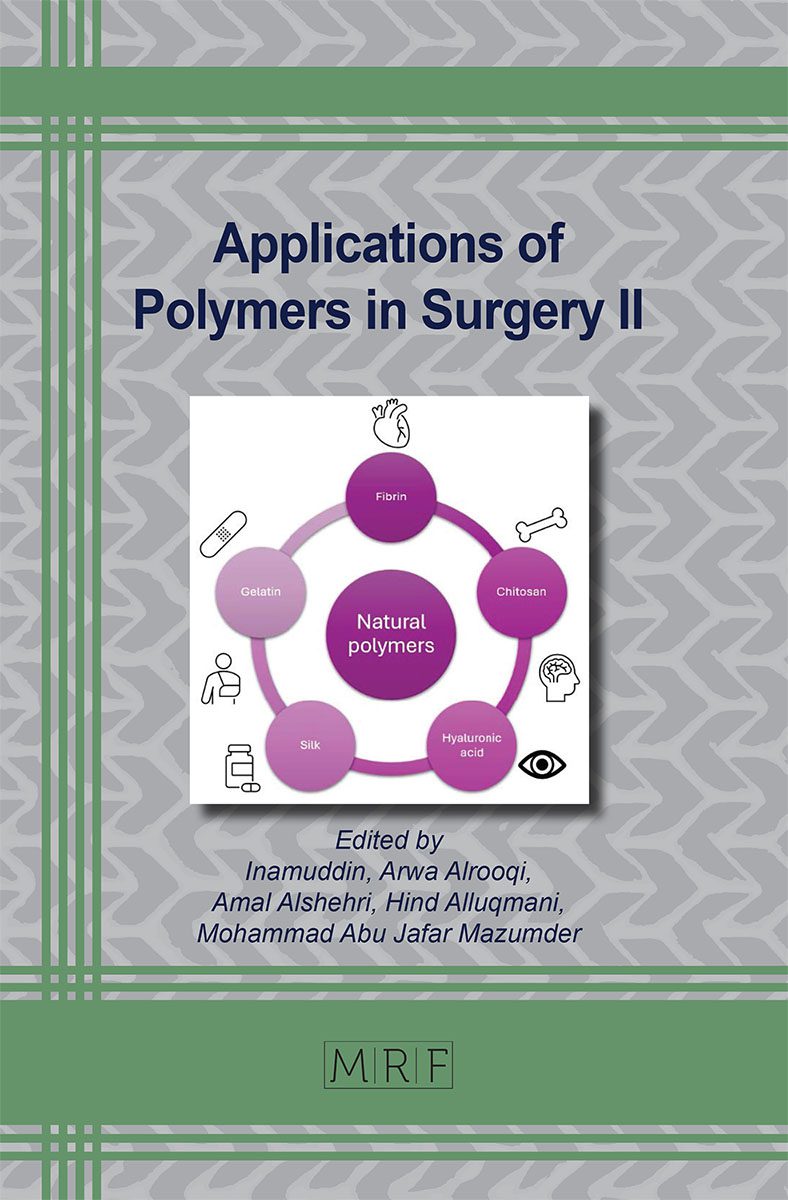
Part of the book on Applications of Polymers in Surgery II
References
[1] B.E.B. Christóforo, D.S. Carvalho, Cuidados de Enfermagem realizados ao paciente cirúrgico no período pré-operatório, Rev. Esc. Enferm. USP. 43 (2009) 14-22. https://doi.org/10.1590/S0080-62342009000100002
[2] M.R. Daian, A. Petroianu, L.R. Alberti, E.E. Jeunon, Estresse em procedimentos cirúrgicos, ABCD Arq. Bras. Cir. Dig. 25 (2012) 118-124. https://doi.org/10.1590/S0102-67202012000200012
[3] J.B.S Garcia, P. Bonilla, D.C. Kraychete, F.C. Flores, E.D.P. de Valtolina, C. Guerrero, Optimizing post-operative pain management in Latin America, Rev. Bras. Anestesiol. 67 (2017) 395-403. https://doi.org/10.1016/j.bjane.2016.04.003
[4] A.D.J. Bombin, N.J. Dunne, H.O Mccarthya, Electrospinning of natural polymers for the production of nanofibres for wound healing applications, Mater. Sci. Eng. C. 114 (2020) 110994. https://doi.org/10.1016/j.msec.2020.110994
[5] H.M Mansour, M. Sohn, A. Al-Ghananeem, P.P. Deluca, Materials for pharmaceutical dosage forms: molecular pharmaceutics and controlled release drug delivery aspects, Int. J. Mol. Sci. 11 (2010) 3298–3322. https://doi.org/10.3390/ijms11093298
[6] J.C.O. Villanova; R.L. Oréfice, S.A. Cunha, Aplicações Farmacêuticas de Polímeros, Polímeros: Ciênc. Tecnol. 20 (2010) 51-64. https://doi.org/10.1590/S0104-14282010005000009
[7] P.J. Sinko, Y. Singh, G.E. Amidon, C.R. Middaugh, H. Omidian, K. Park, T.J. Siahaan, H. Zheng, Martin’s physical pharmacy and pharmaceutical sciences: physical chemical and biopharmaceutical principles in the pharmaceutical sciences, sixth ed., New Jersey, Department of Pharmaceutics Ernest Ernest Mario School of Pharmacy Rutgers, The State University of New Jersey, 2006.
[8] Jr. Canevarolo, V. Sebastião, Ciência dos polímeros, second ed., Artliber Editora, São Paulo, 2002.
[9] P.K Dutta, J. Dutta, V.S Tripathi, Chitin and Chitosan: Chemistry, properties and application. J. Sci. Ind. Res. (2004) 20-31.
[10] H.A Pawar, S.R. Kamat, P.D. Choudhary, An Overview of Natural Polysaccharides as Biological Macromolecules: Their Chemical Modifications and Pharmaceutical Applications. Biol. Med. 7 (2015) 1-9.
[11] S.J. Gautier, J. Lecourtier, Structural characterization by 13C nuclear magnetic resonance of hydrolyzed carboxymethylcellulose, Polym. Bull. 26 (1991) 457- 464.
[12] S.H. Barbanti, C.A.C. Zavaglia, E.A.R. Duek, Polímeros Biorreabsorvíveis como Substrato para Cultura de Células e Engenharia Tecidual. Polímeros: Ciênc. Tecnol. 15 (2005) 13. https://doi.org/10.1590/S0104-14282007000400010
[13] F.C. Carvalho, M.L. Bruschi, R.C. Evangelista, M.P.D. Gremião, Mucoadhesive drug delivery systems. Braz. J. Pharm. Sci. 46 (2010) 2. https://doi.org/10.1590/S1984-82502010000100002
[14] G.P Andrews, T.P Laverty, D.S Jones, Mucoadhesive polymeric platforms for controlled drug delivery. Eur. J. Pharm. Biopharm. 71 (2009) 505. https://doi.org/10.1016/j.ejpb.2008.09.028
[15] N.A. Peppas, P. Bures, W. Leobandung, H. Ichikawa, Hydrogeles in pharmaceutical formulations, Eur. J. Pharm. Biopharm. 50 (2000) 27-46. https://doi.org/10.1016/S0939-6411(00)00090-4
[16] C. Lin, A.T Metters, Hydrogels in controlled release formulations: network design and mathematical modeling, Adv. Drug Delivery Rev. 58 (2006) 1379. https://doi.org/10.1016/j.addr.2006.09.004
[17] O. Pillai, R. Panchagnula, Polymers in drug delivery, Curr. Opin. Chem. Biol. 5 (2001) 447. https://doi.org/10.1016/S1367-5931(00)00227-1
[18] H.G. Börner, H. Schlaad, Bioinspired functional block copolymers. Soft Matter. 3 (2007) 394. https://doi.org/10.1039/B615985K
[19] S. Liu; R. Maheshwari, K.L. Kiick, Polymer-Based Therapeutics, Macromolecules. 42 (2009) 3-13. https://doi.org/10.1021/ma801782q
[20] J.C.O. Villanova, V.R. Sá, Excipientes: guia prático para padronização, LMC – Pharmabooks, São Paulo, 2009.
[21] R.C. Rowe, P. Sheskey, S.C. Owen, Handbook Pharmaceutical Excipients, fifth ed., American Pharmacists Association, Washington, 2006.
[22] M.E. Aulton, Delineamento de formas farmacêuticas, second ed., Artmed, Porto Alegre, 2005.
[23] J. Swarbrick, Encyclopedia of Pharmaceutical Technology, third ed., Informa Healthcare, England, 2007.
[24] S. Mallick; S. Pattnaik; K. Swain, Current perspectives of solubilization: potential for improved bioavailability, Drug Dev. Ind. Pharm. 33 (2007) 865. https://doi.org/10.1080/03639040701429333
[25] T. Tadros, T. Polymeric surfactants in disperse systems, Adv. Colloid Interface Sci. 147 (2009) 281-299. https://doi.org/10.1016/j.cis.2008.10.005
[26] K.L. Kiick, Polymer Therapeutics, Science. 317 (2007) 1182-1183.
[27] A.S. Hoffman, The origins and evolution of “controlled” drug delivery systems, J. Control. Release, 132 (2008) 153. https://doi.org/10.1016/j.jconrel.2008.08.012
[28] W.F. Paterson, E. Mcneil, S. Reis, A.S. Hollmann, M.D.C. Donaldson, Efficacy of Zoladex LA (goserelin) in the treatment of girls with central precocious or early puberty, Arch. Dis. Child. 79 (1988) 323. https://doi.org/10.1136/adc.79.4.323
[29] L.S. Nair & C.T. Laurencin, Biodegradable polymers as biomaterials, Progr. Polym. Sci. 32 (2007) 762. https://doi.org/10.1016/j.progpolymsci.2007.05.017
[30] J. Brady, T. Dürig, P.I. Lee, J.-X. Li, Polymer Properties and Characterization, in: Y. Qiu, Y. Chen, G.G.Z. Zhang, L. Yu, R.V Mantri (Eds.), Developing Solid Oral Dosage Forms: pharmaceutical theory and practice, Academic Press, Massachusetts, 2017, pp. 181-223.
[31] A.T. Pham, P.I. Lee, Probing the mechanism of drug release from hydroxypropyl methylcellulose matrices, Pharm. Res. 11 (1994) 1379-1384. https://doi.org/10.1023/A:1018975318805
[32] P. Gao, J.W. Skoug, P.R. Nixon, T.R. Ju, N.L. Stemm, K.C. Sung, Swelling of hydroxypropyl methylcellulose matrix tablets. 2. Mechanistic study of the influence of formulation variables on matrix performance and drug release, J. Pharm. Sci. 85 (1996) 732-740. https://doi.org/10.1021/js9504595
[33] R. Eyjolfsson, Hydroxypropyl methylcellulose mixtures: effects and kinetics of release of an insoluble drug, Drug Dev. Ind. Pharm. 25 (1999) 667-669. https://doi.org/10.1081/DDC-100102223
[34] M.N.V. Ravi Kumar, N. Kumar, Polymeric controlled drug-delivery systems: perspective issues and opportunities, Drug Dev. Ind. Pharm. 27 (2001) 1-30. https://doi.org/10.1081/DDC-100000124
[35] M.E. Aulton, Pharmaceutics: The science of dosage form design, second ed., Churchill Livingstone, Edinburgh, 2002.
[36] P.R. Petrovick, E.C. Lopes, Emprego da ultrafiltração na análise do ambroxol. UFRGS, Porto Alegre, 1993.
[37] L.V. Allen, N.G. Popovich, H.C. Ansel, Ansel’s pharmaceutical dosage forms, ninth ed., Lippincott Williams & Wilkins, Philadelphia, 2005.
[38] W. Gunder, B.H. Lippold, B.C. Lippold, Release of drugs from ethyl cellulose microcapsules (diffusion pellets) with pore formers and pore fusion, Eur. J. Pharm. Sci. 3 (1995) 203–214. https://doi.org/10.1016/0928-0987(95)00009-3
[39] R.B. Oliveira, E.M. Lima, Polímeros na obtenção de sistemas de liberação de fármacos, Rev. Eletrôn. Farm. 3 (2006) 29-35.
[40] P. Burey, B.R. Bhandari, T. Howes, M.J. Gidley, Hydrocolloid gel particles: formation, characterization, and application, Crit. Rev. Food Sci. Nutr. 48 (2008) 361-377. https://doi.org/10.1080/10408390701347801
[41] J. Milani, G. Maleki, Hydrocolloids in Food Industry, in: B. Valdez (Ed.), Food Industrial Processes – Methods and Equipment, BoD-Books on Demand, Norderstedt, 2012, pp. 18-22.
[42] S.P. Vyas, R.K. Khar, Controlled Drug Delivery: Concepts and Advances, first. ed., Vallabh Prakashan, Dehli, 2002.
[43] T.K. Giri, Alginate Containing Nanoarchitectonics for Improved Cancer Therapy, in: A.M. Holban, A.M. Grumezescu (Eds.), Nanoarchitectonics for Smart Delivery and Drug Targeting, William Andrew Publishing, Norwich, 2016, pp. 565-588. https://doi.org/10.1016/B978-0-323-47347-7.00020-3
[44] O. Felt, P. Buri, R. Gurny, Chitosan: a unique polysaccharide for drug delivery, Drug Dev. Ind. Pharm. 24 (1998) 979–993. https://doi.org/10.3109/03639049809089942
[45] A. K. Singla, M. Chawla, Chitosan: some pharmaceutical and biological aspects, J. Pharm. Pharmacol. 53 (2001) 1047–1067. https://doi.org/10.1211/0022357011776441
[46] B. Singh, S. Maharjan, K-H. Cho, L. Cui, I-K Park, Y-J. Choi, C-S. Cho, Chitosan-based particulate systems for the delivery of mucosal vaccines against infectious diseases, Int. J. Biol. Macromol. 110 (2018) 54-64. https://doi.org/10.1016/j.ijbiomac.2017.10.101
[47] A. Binello, G. Crabotto, G.M. Nano, P. Spagliardi, Synthesis of chitosan–cyclodextrin adducts and evaluation of their bitter-masking properties, Flavour Fragr. J. 19 (2004) 394-400. https://doi.org/10.1002/ffj.1434
[48] L. Kudsiova, M.J. Lawrence, A comparison of the effect of chitosan and chitosan-coated vesicles on monolayer integrity and permeability across Caco-2 and 16HBE14o-cells, J. Pharm. Sci. 97 (2008) 3998-4010. https://doi.org/10.1002/jps.21262
[49] J. Potaś, E. Szymańska, K. Winnicka, Challenges in developing of chitosan – Based polyelectrolyte complexes as a platform for mucosal and skin drug delivery, Eur. Polym. J. 140 (2020) 1-11. https://doi.org/10.1016/j.eurpolymj.2020.110020
[50] S. Y. Yu, J. Hu, X. Pan, P. Yao, M. Jiang, Stable and pH-sensitive nanogels prepared by self-assembly of chitosan and ovalbumin, Langmuir. 22(2006) 2754–2759. https://doi.org/10.1021/la053158b
[51] S. Senel, S. J. McClure, Potential applications of chitosan in veterinary medicine, Adv. Drug Deliv. Rev. 56 (2004) 1467–1480. https://doi.org/10.1016/j.addr.2004.02.007
[52] M. Thanou, J. C. Verhoef and H. E. Junginger, Oral drug absorption enhancement by chitosan and its derivatives, Adv. Drug Deliv. Rev. 52 (2001) 117–126. https://doi.org/10.1016/S0169-409X(01)00231-9
[53] J. Grant, J. Cho and C. Allen, Self-assembly and physicochemical and rheological properties of a polysaccharide−surfactant system formed from the cationic biopolymer chitosan and nonionic sorbitan esters, Langmuir. 22 (2006) 4327–4335. https://doi.org/10.1021/la7004166
[54] T. Dai, M. Tanaka, Y. Huang, M.R. Hamblin, Chitosan preparations for wounds & burns: antimicrobial & wound-healing effects, Expert. Rev. Anti Infect. Ther. 9 (2011) 857–879. https://doi.org/10.1586/eri.11.59
[55] E. Wan, E. Galembeck, F. Galembeck, Polímeros sintéticos, in: Química Nova na Escola, PubliSBQ, São Paulo, 2001, pp. 5-8.
[56] E.A. Slatopolsky, S.K. Burke, M.A. Dillon, RenaGel, a nonabsorbed calcium- and aluminum-free phosphate binder, lowers serum phosphorus and parathyroid hormone, Kidney Int. 55 (1999) 299-306. https://doi.org/10.1046/j.1523-1755.1999.00240.x
[57] R.G. Strickley, Solubilizing excipients in oral and injectable formulations, Pharm. Res. 21 (2004) 201. https://doi.org/10.1023/B:PHAM.0000016235.32639.23
[58] A. Franzol, M.C. Rezende, Estabilidade de emulsões: um estudo de caso envolvendo emulsionantes aniônico, catiônico e não-iônico. Polímeros. 25 (2015) 1-9. https://doi.org/10.1590/0104-1428.1669.
[59] Brasil. Agência Nacional de Vigilância Sanitária. Brasília: ANVISA. Farmacopeia Brasileira, volume 2, 2010.
[60] CosmeticsOnline, Fundamentos da Cosmetologia – Cremes e Loções Cosmetics, https://www.cosmeticsonline.com.br/artigo/81 (accessed 20 May 2024).
[61] CosmeticsOnline, Fundamentos da Cosmetologia – Géis Cosméticos, https://www.cosmeticsonline.com.br/artigo/83 (accessed 20 May 2024).
[62] A.M.S Sawamura, S.L. Franco, Sistemas Terapêuticos Transdérmicos, Arquivos de Mudi. 8 (2012) 1-8.
[63] A.R. Gennaro, Remington: the science and practice of pharmacy, Lippincott Williams e Wilkins, Philadelphia, 2006.
[64] M.R. Prausnitz, R. Langer. Transdermal drug delivery. Nat. Biotechnol. 11 (2008) 1261-1268. https://doi.org/10.1038/nbt.1504.
[65] I.D Miziara, O uso da antibioticoterapia no tratamento das doenças bucais, JBC. 2 (1998) 57-67.
[66] F.R.G Seabra, B.G.M Seabra, E.G. Seabra, Antibioticoterapia profilática em cirurgias periodontais, Odont. Clín. Cient. 3 (2004) 11-16.
[67] T.C. Woods, A.R. Marks, Drug-eluting stents, Annu. Rev. Med. 55 (2004) 169-178. https://doi.org/10.1146/annurev.med.55.091902.105243
[68] R. Ghadi, A. Jain, W. Khan, A.J. Domb, Microparticulate polymers and hydrogels for wound healing, in: M.S. Ågren (Ed.), Wound Healing Biomaterials, Woodhead Publishing, 2016, pp. 203-25.
[69] D. Stern, H. Cui, Crafting polymeric and peptidic hydrogels for improved wound healing, Adv. Healthc. Mater. 8 (2019). https://doi.org/10.1002/adhm.201900104
[70] Y. Kang, J. Kim, Y. Mi Lee, S.S. Kim; H. Park, W.J. Kim, Nitric oxide-releasing polymer incorporated ointment for cutaneous wound healing, J. Control. Release. 220 (2015) 624-630. https://doi.org/10.1016/j.jconrel.2015.08.057