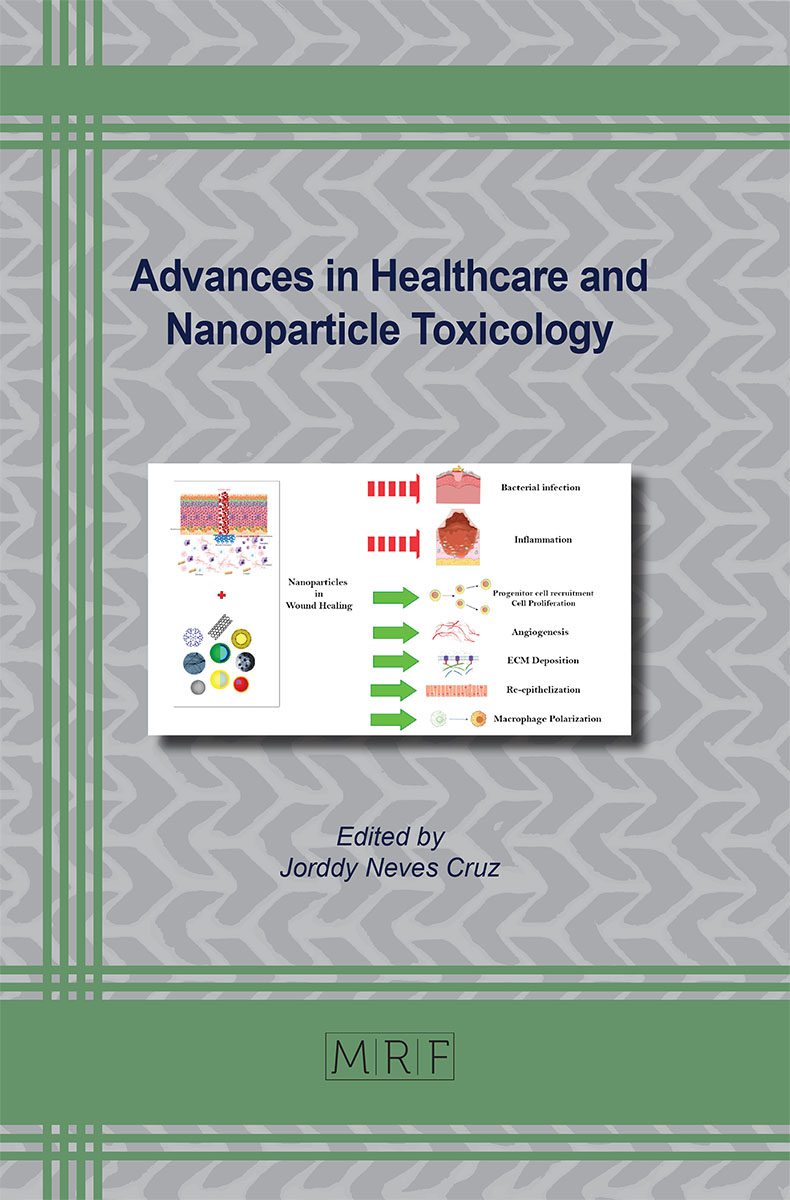
Whispers of Healing: Navigation of Nanomaterials for Wound Restoration and Inflammation Control
Nameeta Jesudoss M., Cannon Antony Fernandes, Joddy Neves Cruz, Vasantha Veerappa Lakshmaiah
Impaired healing in chronic wounds is associated with an upsurge in financial burden for treatment, high mortality rates and limited availability of medicinal resources which mounts a burden on the global healthcare system. The major challenges associated with wounds are the absence of suitable microenvironment to facilitate the migration of cells and angiogenesis, microbial infection at the wound site and aggressive inflammation. The existing treatment strategies have failed to combat these challenges and aid in faster healing of the wounds. In an effort to address these challenges, recent studies prove the use of the unique advantages of nanomaterials towards effective wound healing. Integration of nanomaterials into the current therapeutic approaches has the potential to induce the required molecular and cellular process to create an amiable microenvironment for wound healing through its anti-bacterial, anti-inflammatory properties and angiogenic effects. This review highlights the pathophysiology of wound healing and the recent findings and challenges pertaining to the use of nanomaterials towards chronic wound management.
Keywords
Chronic Wounds, Nanomaterials, Inflammation, Angiogenesis, Infection, Healing Mechanism
Published online 12/15/2024, 42 pages
Citation: Nameeta Jesudoss M., Cannon Antony Fernandes, Joddy Neves Cruz, Vasantha Veerappa Lakshmaiah, Whispers of Healing: Navigation of Nanomaterials for Wound Restoration and Inflammation Control, Materials Research Foundations, Vol. 171, pp 93-134, 2024
DOI: https://doi.org/10.21741/9781644903339-4
Part of the book on Advances in Healthcare and Nanoparticle Toxicology
References
[1] D.G. Armstrong, J. Wrobel, J.M. Robbins, Guest Editorial: are diabetes-related wounds and amputations worse than cancer?, Int Wound J 4 (2007) 286–287. https://doi.org/10.1111/j.1742-481X.2007.00392.x.
[2] A. Clinton, T. Carter, Chronic Wound Biofilms: Pathogenesis and Potential Therapies, Lab Med 46 (2015) 277–284. https://doi.org/10.1309/LMBNSWKUI4JPN7SO.
[3] R.K. Thapa, K.L. Kiick, M.O. Sullivan, Encapsulation of collagen mimetic peptide-tethered vancomycin liposomes in collagen-based scaffolds for infection control in wounds, Acta Biomater 103 (2020) 115–128. https://doi.org/10.1016/j.actbio.2019.12.014.
[4] N. Monteiro, M. Martins, A. Martins, N.A. Fonseca, J.N. Moreira, R.L. Reis, N.M. Neves, Antibacterial activity of chitosan nanofiber meshes with liposomes immobilized releasing gentamicin, Acta Biomater 18 (2015) 196–205. https://doi.org/10.1016/j.actbio.2015.02.018.
[5] S. Ellis, E.J. Lin, D. Tartar, Immunology of Wound Healing, Curr Dermatol Rep 7 (2018) 350–358. https://doi.org/10.1007/s13671-018-0234-9.
[6] G. Hosgood, Stages of Wound Healing and Their Clinical Relevance, Veterinary Clinics of North America: Small Animal Practice 36 (2006) 667–685. https://doi.org/10.1016/j.cvsm.2006.02.006.
[7] G. Gethin, Understanding the inflammatory process in wound healing, Br J Community Nurs 17 (2012) S17–S22. https://doi.org/10.12968/bjcn.2012.17.Sup3.S17.
[8] J. Li, J. Chen, R. Kirsner, Pathophysiology of acute wound healing, Clin Dermatol 25 (2007) 9–18. https://doi.org/10.1016/j.clindermatol.2006.09.007.
[9] A.C. de O. Gonzalez, T.F. Costa, Z. de A. Andrade, A.R.A.P. Medrado, Wound healing – A literature review, An Bras Dermatol 91 (2016) 614–620. https://doi.org/10.1590/abd1806-4841.20164741.
[10] T.N. Demidova-Rice, M.R. Hamblin, I.M. Herman, Acute and Impaired Wound Healing, Adv Skin Wound Care 25 (2012) 304–314. https://doi.org/10.1097/01.ASW.0000416006.55218.d0.
[11] L.F. Rose, R.K. Chan, The Burn Wound Microenvironment, Adv Wound Care (New Rochelle) 5 (2016) 106–118. https://doi.org/10.1089/wound.2014.0536.
[12] S. Barrientos, H. Brem, O. Stojadinovic, M. Tomic-Canic, Clinical application of growth factors and cytokines in wound healing, Wound Repair and Regeneration 22 (2014) 569–578. https://doi.org/10.1111/wrr.12205.
[13] P. Olczyk, Ł. Mencner, K. Komosinska-Vassev, Diverse Roles of Heparan Sulfate and Heparin in Wound Repair, Biomed Res Int 2015 (2015) 1–7. https://doi.org/10.1155/2015/549417.
[14] S. Barrientos, O. Stojadinovic, M.S. Golinko, H. Brem, M. Tomic-Canic, PERSPECTIVE ARTICLE: Growth factors and cytokines in wound healing, Wound Repair and Regeneration 16 (2008) 585–601. https://doi.org/10.1111/j.1524-475X.2008.00410.x.
[15] R.D. Burgoyne, A. Morgan, Secretory Granule Exocytosis, Physiol Rev 83 (2003) 581–632. https://doi.org/10.1152/physrev.00031.2002.
[16] S. Muzammil, J. Neves Cruz, R. Mumtaz, I. Rasul, S. Hayat, M.A. Khan, A.M. Khan, M.U. Ijaz, R.R. Lima, M. Zubair, Effects of Drying Temperature and Solvents on In Vitro Diabetic Wound Healing Potential of Moringa oleifera Leaf Extracts, Molecules 28 (2023). https://doi.org/10.3390/molecules28020710.
[17] G. Gainza, S. Villullas, J.L. Pedraz, R.M. Hernandez, M. Igartua, Advances in drug delivery systems (DDSs) to release growth factors for wound healing and skin regeneration, Nanomedicine 11 (2015) 1551–1573. https://doi.org/10.1016/j.nano.2015.03.002.
[18] N.B. Menke, K.R. Ward, T.M. Witten, D.G. Bonchev, R.F. Diegelmann, Impaired wound healing, Clin Dermatol 25 (2007) 19–25. https://doi.org/10.1016/j.clindermatol.2006.12.005.
[19] S. Barrientos, O. Stojadinovic, M.S. Golinko, H. Brem, M. Tomic-Canic, PERSPECTIVE ARTICLE: Growth factors and cytokines in wound healing, Wound Repair and Regeneration 16 (2008) 585–601. https://doi.org/10.1111/j.1524-475X.2008.00410.x.
[20] P. Wee, Z. Wang, Epidermal Growth Factor Receptor Cell Proliferation Signaling Pathways, Cancers (Basel) 9 (2017) 52. https://doi.org/10.3390/cancers9050052.
[21] Y. Zhao, A.A. Adjei, Targeting Angiogenesis in Cancer Therapy: Moving Beyond Vascular Endothelial Growth Factor, Oncologist 20 (2015) 660–673. https://doi.org/10.1634/theoncologist.2014-0465.
[22] K. Hyldig, S. Riis, C. Pennisi, V. Zachar, T. Fink, Implications of Extracellular Matrix Production by Adipose Tissue-Derived Stem Cells for Development of Wound Healing Therapies, Int J Mol Sci 18 (2017) 1167. https://doi.org/10.3390/ijms18061167.
[23] M.B. Dreifke, A.A. Jayasuriya, A.C. Jayasuriya, Current wound healing procedures and potential care, Materials Science and Engineering: C 48 (2015) 651–662. https://doi.org/10.1016/j.msec.2014.12.068.
[24] J. Larouche, S. Sheoran, K. Maruyama, M.M. Martino, Immune Regulation of Skin Wound Healing: Mechanisms and Novel Therapeutic Targets, Adv Wound Care (New Rochelle) 7 (2018) 209–231. https://doi.org/10.1089/wound.2017.0761.
[25] J. Domínguez-Bendala, L. Inverardi, C. Ricordi, Regeneration of pancreatic beta-cell mass for the treatment of diabetes, Expert Opin Biol Ther 12 (2012) 731–741. https://doi.org/10.1517/14712598.2012.679654.
[26] G.S. Schultz, A. Wysocki, Interactions between extracellular matrix and growth factors in wound healing, Wound Repair and Regeneration 17 (2009) 153–162. https://doi.org/10.1111/j.1524-475X.2009.00466.x.
[27] M. Xue, C.J. Jackson, Extracellular Matrix Reorganization During Wound Healing and Its Impact on Abnormal Scarring, Adv Wound Care (New Rochelle) 4 (2015) 119–136. https://doi.org/10.1089/wound.2013.0485.
[28] M.F. Brizzi, G. Tarone, P. Defilippi, Extracellular matrix, integrins, and growth factors as tailors of the stem cell niche, Curr Opin Cell Biol 24 (2012) 645–651. https://doi.org/10.1016/j.ceb.2012.07.001.
[29] A. Opneja, S. Kapoor, E.X. Stavrou, Contribution of platelets, the coagulation and fibrinolytic systems to cutaneous wound healing, Thromb Res 179 (2019) 56–63. https://doi.org/10.1016/j.thromres.2019.05.001.
[30] C.M. Murphy, M.G. Haugh, F.J. O’Brien, The effect of mean pore size on cell attachment, proliferation and migration in collagen–glycosaminoglycan scaffolds for bone tissue engineering, Biomaterials 31 (2010) 461–466. https://doi.org/10.1016/j.biomaterials.2009.09.063.
[31] P. Rousselle, F. Braye, G. Dayan, Re-epithelialization of adult skin wounds: Cellular mechanisms and therapeutic strategies, Adv Drug Deliv Rev 146 (2019) 344–365. https://doi.org/10.1016/j.addr.2018.06.019.
[32] R.B. Diller, A.J. Tabor, The Role of the Extracellular Matrix (ECM) in Wound Healing: A Review, Biomimetics 7 (2022) 87. https://doi.org/10.3390/biomimetics7030087.
[33] C.S. Oliver Cassell, O.P. Stefan Hofer, W.A. Morrison, K.R. Knight, Vascularisation of tissue-engineered grafts: the regulation of angiogenesis in reconstructive surgery and in disease states, Br J Plast Surg 55 (2002) 603–610. https://doi.org/10.1054/bjps.2002.3950.
[34] A.D. Theocharis, D. Manou, N.K. Karamanos, The extracellular matrix as a multitasking player in disease, FEBS J 286 (2019) 2830–2869. https://doi.org/10.1111/febs.14818.
[35] C. Walker, E. Mojares, A. del Río Hernández, Role of Extracellular Matrix in Development and Cancer Progression, Int J Mol Sci 19 (2018) 3028. https://doi.org/10.3390/ijms19103028.
[36] J.D. Humphrey, E.R. Dufresne, M.A. Schwartz, Mechanotransduction and extracellular matrix homeostasis, Nat Rev Mol Cell Biol 15 (2014) 802–812. https://doi.org/10.1038/nrm3896.
[37] G.S. Schultz, A. Wysocki, Interactions between extracellular matrix and growth factors in wound healing, Wound Repair and Regeneration 17 (2009) 153–162. https://doi.org/10.1111/j.1524-475X.2009.00466.x.
[38] R.B. Diller, A.J. Tabor, The Role of the Extracellular Matrix (ECM) in Wound Healing: A Review, Biomimetics 7 (2022) 87. https://doi.org/10.3390/biomimetics7030087.
[39] M. KJÆR, Role of Extracellular Matrix in Adaptation of Tendon and Skeletal Muscle to Mechanical Loading, Physiol Rev 84 (2004) 649–698. https://doi.org/10.1152/physrev.00031.2003.
[40] A.L. Berrier, K.M. Yamada, Cell–matrix adhesion, J Cell Physiol 213 (2007) 565–573. https://doi.org/10.1002/jcp.21237.
[41] A. Baroni, E. Buommino, V. De Gregorio, E. Ruocco, V. Ruocco, R. Wolf, Structure and function of the epidermis related to barrier properties, Clin Dermatol 30 (2012) 257–262. https://doi.org/10.1016/j.clindermatol.2011.08.007.
[42] J.F. Almine, S.G. Wise, A.S. Weiss, Elastin signaling in wound repair, Birth Defects Res C Embryo Today 96 (2012) 248–257. https://doi.org/10.1002/bdrc.21016.
[43] S. Barrientos, O. Stojadinovic, M.S. Golinko, H. Brem, M. Tomic-Canic, PERSPECTIVE ARTICLE: Growth factors and cytokines in wound healing, Wound Repair and Regeneration 16 (2008) 585–601. https://doi.org/10.1111/j.1524-475X.2008.00410.x.
[44] B.M. Delavary, W.M. van der Veer, M. van Egmond, F.B. Niessen, R.H.J. Beelen, Macrophages in skin injury and repair, Immunobiology 216 (2011) 753–762. https://doi.org/10.1016/j.imbio.2011.01.001.
[45] M. Fioranelli, M.G. Roccia, D. Flavin, L. Cota, Regulation of Inflammatory Reaction in Health and Disease, Int J Mol Sci 22 (2021) 5277. https://doi.org/10.3390/ijms22105277.
[46] A. Yang, Y. Wu, G. Yu, H. Wang, Role of specialized pro-resolving lipid mediators in pulmonary inflammation diseases: mechanisms and development, Respir Res 22 (2021) 204. https://doi.org/10.1186/s12931-021-01792-y.
[47] G. Fredman, N. Kamaly, S. Spolitu, J. Milton, D. Ghorpade, R. Chiasson, G. Kuriakose, M. Perretti, O. Farokhzad, I. Tabas, Targeted nanoparticles containing the proresolving peptide Ac2-26 protect against advanced atherosclerosis in hypercholesterolemic mice, Sci Transl Med 7 (2015). https://doi.org/10.1126/scitranslmed.aaa1065.
[48] E.H. Steen, X. Wang, S. Balaji, M.J. Butte, P.L. Bollyky, S.G. Keswani, The Role of the Anti-Inflammatory Cytokine Interleukin-10 in Tissue Fibrosis, Adv Wound Care (New Rochelle) 9 (2020) 184–198. https://doi.org/10.1089/wound.2019.1032.
[49] K. Zhang, V.C.H. Lui, Y. Chen, C.N. Lok, K.K.Y. Wong, Delayed application of silver nanoparticles reveals the role of early inflammation in burn wound healing, Sci Rep 10 (2020) 6338. https://doi.org/10.1038/s41598-020-63464-z.
[50] S.M. Hirst, A.S. Karakoti, R.D. Tyler, N. Sriranganathan, S. Seal, C.M. Reilly, Anti-inflammatory Properties of Cerium Oxide Nanoparticles, Small 5 (2009) 2848–2856. https://doi.org/10.1002/smll.200901048.
[51] Y. Wu, Y. Yang, W. Zhao, Z.P. Xu, P.J. Little, A.K. Whittaker, R. Zhang, H.T. Ta, Novel iron oxide–cerium oxide core–shell nanoparticles as a potential theranostic material for ROS related inflammatory diseases, J Mater Chem B 6 (2018) 4937–4951. https://doi.org/10.1039/C8TB00022K.
[52] Z. Zhai, W. Ouyang, Y. Yao, Y. Zhang, H. Zhang, F. Xu, C. Gao, Dexamethasone-loaded ROS-responsive poly(thioketal) nanoparticles suppress inflammation and oxidative stress of acute lung injury, Bioact Mater 14 (2022) 430–442. https://doi.org/10.1016/j.bioactmat.2022.01.047.
[53] T. Yu, S. Gan, Q. Zhu, D. Dai, N. Li, H. Wang, X. Chen, D. Hou, Y. Wang, Q. Pan, J. Xu, X. Zhang, J. Liu, S. Pei, C. Peng, P. Wu, S. Romano, C. Mao, M. Huang, X. Zhu, K. Shen, J. Qin, Y. Xiao, Modulation of M2 macrophage polarization by the crosstalk between Stat6 and Trim24, Nat Commun 10 (2019) 4353. https://doi.org/10.1038/s41467-019-12384-2.
[54] H. Yen, S. Hsu, C. Tsai, Cytotoxicity and Immunological Response of Gold and Silver Nanoparticles of Different Sizes, Small 5 (2009) 1553–1561. https://doi.org/10.1002/smll.200900126.
[55] S. Zanganeh, G. Hutter, R. Spitler, O. Lenkov, M. Mahmoudi, A. Shaw, J.S. Pajarinen, H. Nejadnik, S. Goodman, M. Moseley, L.M. Coussens, H.E. Daldrup-Link, Iron oxide nanoparticles inhibit tumour growth by inducing pro-inflammatory macrophage polarization in tumour tissues, Nat Nanotechnol 11 (2016) 986–994. https://doi.org/10.1038/nnano.2016.168.
[56] Y. Yang, L. Guo, Z. Wang, P. Liu, X. Liu, J. Ding, W. Zhou, Targeted silver nanoparticles for rheumatoid arthritis therapy via macrophage apoptosis and Re-polarization, Biomaterials 264 (2021) 120390. https://doi.org/10.1016/j.biomaterials.2020.120390.
[57] M. Sun, Z. Deng, F. Shi, Z. Zhou, C. Jiang, Z. Xu, X. Cui, W. Li, Y. Jing, B. Han, W. Zhang, S. Xia, Rebamipide-loaded chitosan nanoparticles accelerate prostatic wound healing by inhibiting M1 macrophage-mediated inflammation via the NF-κB signaling pathway, Biomater Sci 8 (2020) 912–925. https://doi.org/10.1039/C9BM01512D.
[58] D. Kwon, B.G. Cha, Y. Cho, J. Min, E.-B. Park, S.-J. Kang, J. Kim, Extra-Large Pore Mesoporous Silica Nanoparticles for Directing in Vivo M2 Macrophage Polarization by Delivering IL-4, Nano Lett 17 (2017) 2747–2756. https://doi.org/10.1021/acs.nanolett.6b04130.
[59] L. Wang, H. Zhang, L. Sun, W. Gao, Y. Xiong, A. Ma, X. Liu, L. Shen, Q. Li, H. Yang, Manipulation of macrophage polarization by peptide-coated gold nanoparticles and its protective effects on acute lung injury, J Nanobiotechnology 18 (2020) 38. https://doi.org/10.1186/s12951-020-00593-7.
[60] L. Kou, H. Huang, Y. Tang, M. Sun, Y. Li, J. Wu, S. Zheng, X. Zhao, D. Chen, Z. Luo, X. Zhang, Q. Yao, R. Chen, Opsonized nanoparticles target and regulate macrophage polarization for osteoarthritis therapy: A trapping strategy, Journal of Controlled Release 347 (2022) 237–255. https://doi.org/10.1016/j.jconrel.2022.04.037.
[61] M. Mittal, M.R. Siddiqui, K. Tran, S.P. Reddy, A.B. Malik, Reactive Oxygen Species in Inflammation and Tissue Injury, Antioxid Redox Signal 20 (2014) 1126–1167. https://doi.org/10.1089/ars.2012.5149.
[62] D. Martinvalet, M. Walch, Editorial: The Role of Reactive Oxygen Species in Protective Immunity, Front Immunol 12 (2022). https://doi.org/10.3389/fimmu.2021.832946.
[63] Y. Ranneh, F. Ali, A.M. Akim, H.Abd. Hamid, H. Khazaai, A. Fadel, Crosstalk between reactive oxygen species and pro-inflammatory markers in developing various chronic diseases: a review, Appl Biol Chem 60 (2017) 327–338. https://doi.org/10.1007/s13765-017-0285-9.
[64] M. Mittal, M.R. Siddiqui, K. Tran, S.P. Reddy, A.B. Malik, Reactive oxygen species in inflammation and tissue injury., Antioxid Redox Signal 20 (2014) 1126–67. https://doi.org/10.1089/ars.2012.5149.
[65] S. Watanabe, M. Alexander, A. V. Misharin, G.R.S. Budinger, The role of macrophages in the resolution of inflammation, Journal of Clinical Investigation 129 (2019) 2619–2628. https://doi.org/10.1172/JCI124615.
[66] M.V.D.Z. Park, A.M. Neigh, J.P. Vermeulen, L.J.J. de la Fonteyne, H.W. Verharen, J.J. Briedé, H. van Loveren, W.H. de Jong, The effect of particle size on the cytotoxicity, inflammation, developmental toxicity and genotoxicity of silver nanoparticles, Biomaterials 32 (2011) 9810–9817. https://doi.org/10.1016/j.biomaterials.2011.08.085.
[67] E.-J. Park, K. Park, Oxidative stress and pro-inflammatory responses induced by silica nanoparticles in vivo and in vitro, Toxicol Lett 184 (2009) 18–25. https://doi.org/10.1016/j.toxlet.2008.10.012.
[68] R.P. Nishanth, R.G. Jyotsna, J.J. Schlager, S.M. Hussain, P. Reddanna, Inflammatory responses of RAW 264.7 macrophages upon exposure to nanoparticles: Role of ROS-NFκB signaling pathway, Nanotoxicology 5 (2011) 502–516. https://doi.org/10.3109/17435390.2010.541604.
[69] L. Sui, J. Wang, Z. Xiao, Y. Yang, Z. Yang, K. Ai, ROS-Scavenging Nanomaterials to Treat Periodontitis, Front Chem 8 (2020). https://doi.org/10.3389/fchem.2020.595530.
[70] Q. Li, Y. Liu, X. Dai, W. Jiang, H. Zhao, Nanozymes Regulate Redox Homeostasis in ROS-Related Inflammation, Front Chem 9 (2021). https://doi.org/10.3389/fchem.2021.740607.
[71] S. Zhao, Y. Li, Q. Liu, S. Li, Y. Cheng, C. Cheng, Z. Sun, Y. Du, C.J. Butch, H. Wei, An Orally Administered CeO 2 @Montmorillonite Nanozyme Targets Inflammation for Inflammatory Bowel Disease Therapy, Adv Funct Mater 30 (2020) 2004692. https://doi.org/10.1002/adfm.202004692.
[72] R. Li, X. Hou, L. Li, J. Guo, W. Jiang, W. Shang, Application of Metal-Based Nanozymes in Inflammatory Disease: A Review., Front Bioeng Biotechnol 10 (2022) 920213. https://doi.org/10.3389/fbioe.2022.920213.
[73] N. Singh, M.A. Savanur, S. Srivastava, P. D’Silva, G. Mugesh, A Redox Modulatory Mn 3 O 4 Nanozyme with Multi-Enzyme Activity Provides Efficient Cytoprotection to Human Cells in a Parkinson’s Disease Model, Angewandte Chemie International Edition 56 (2017) 14267–14271. https://doi.org/10.1002/anie.201708573.
[74] J. Yao, Y. Cheng, M. Zhou, S. Zhao, S. Lin, X. Wang, J. Wu, S. Li, H. Wei, ROS scavenging Mn 3 O 4 nanozymes for in vivo anti-inflammation, Chem Sci 9 (2018) 2927–2933. https://doi.org/10.1039/C7SC05476A.
[75] C. Xu, O.U. Akakuru, X. Ma, J. Zheng, J. Zheng, A. Wu, Nanoparticle-Based Wound Dressing: Recent Progress in the Detection and Therapy of Bacterial Infections, Bioconjug Chem 31 (2020) 1708–1723. https://doi.org/10.1021/acs.bioconjchem.0c00297.
[76] M. Ahamed, M.S. AlSalhi, M.K.J. Siddiqui, Silver nanoparticle applications and human health, Clinica Chimica Acta 411 (2010) 1841–1848. https://doi.org/10.1016/j.cca.2010.08.016.
[77] J.N. Cruz, S. Muzammil, A. Ashraf, M.U. Ijaz, M.H. Siddique, R. Abbas, M. Sadia, Saba, S. Hayat, R.R. Lima, A review on mycogenic metallic nanoparticles and their potential role as antioxidant, antibiofilm and quorum quenching agents, Heliyon 10 (2024). https://doi.org/10.1016/j.heliyon.2024.e29500.
[78] X.-F. Zhang, Z.-G. Liu, W. Shen, S. Gurunathan, Silver Nanoparticles: Synthesis, Characterization, Properties, Applications, and Therapeutic Approaches, Int J Mol Sci 17 (2016) 1534. https://doi.org/10.3390/ijms17091534.
[79] A. Kędziora, M. Speruda, E. Krzyżewska, J. Rybka, A. Łukowiak, G. Bugla-Płoskońska, Similarities and Differences between Silver Ions and Silver in Nanoforms as Antibacterial Agents, Int J Mol Sci 19 (2018) 444. https://doi.org/10.3390/ijms19020444.
[80] M. Konop, J. Czuwara, E. Kłodzińska, A.K. Laskowska, D. Sulejczak, T. Damps, U. Zielenkiewicz, I. Brzozowska, A. Sureda, T. Kowalkowski, R.A. Schwartz, L. Rudnicka, Evaluation of keratin biomaterial containing silver nanoparticles as a potential wound dressing in full‐thickness skin wound model in diabetic mice, J Tissue Eng Regen Med 14 (2020) 334–346. https://doi.org/10.1002/term.2998.
[81] M. Ruiz-Serrano, J.C. Menéndez, Multicomponent reactions for the synthesis of natural products and natural product-like libraries, in: J.N. Cruz (Ed.), Drug Discovery and Design Using Natural Products, Springer Nature Switzerland, Cham, 2023: pp. 273–322. https://doi.org/10.1007/978-3-031-35205-8_10.
[82] G.A. Govindasamy, R.B. S. M. N. Mydin, W.N.F.W.E. Effendy, S. Sreekantan, Novel dual-ionic ZnO/CuO embedded in porous chitosan biopolymer for wound dressing application: Physicochemical, bactericidal, cytocompatibility and wound healing profiles, Mater Today Commun 33 (2022) 104545. https://doi.org/10.1016/j.mtcomm.2022.104545.
[83] M.I.N. Ahamed, S. Sankar, P.M. Kashif, S.K.H. Basha, T.P. Sastry, Evaluation of biomaterial containing regenerated cellulose and chitosan incorporated with silver nanoparticles, Int J Biol Macromol 72 (2015) 680–686. https://doi.org/10.1016/j.ijbiomac.2014.08.055.
[84] Z. Qian, Y. Bai, J. Zhou, L. Li, J. Na, Y. Fan, X. Guo, H. Liu, A moisturizing chitosan-silk fibroin dressing with silver nanoparticles-adsorbed exosomes for repairing infected wounds, J Mater Chem B 8 (2020) 7197–7212. https://doi.org/10.1039/D0TB01100B.
[85] I.N. de F. Ramos, M.F. da Silva, J.M.S. Lopes, J.N. Cruz, F.S. Alves, J. de A.R. do Rego, M.L. da Costa, P.P. de Assumpção, D. do S. Barros Brasil, A.S. Khayat, Extraction, Characterization, and Evaluation of the Cytotoxic Activity of Piperine in Its Isolated form and in Combination with Chemotherapeutics against Gastric Cancer, Molecules 28 (2023). https://doi.org/10.3390/molecules28145587.
[86] N. Tra Thanh, M. Ho Hieu, N. Tran Minh Phuong, T. Do Bui Thuan, H. Nguyen Thi Thu, V.P. Thai, T. Do Minh, H. Nguyen Dai, V.T. Vo, H. Nguyen Thi, Optimization and characterization of electrospun polycaprolactone coated with gelatin-silver nanoparticles for wound healing application, Materials Science and Engineering: C 91 (2018) 318–329. https://doi.org/10.1016/j.msec.2018.05.039.
[87] M. Konop, E. Kłodzińska, J. Borowiec, A.K. Laskowska, J. Czuwara, P. Konieczka, B. Cieślik, E. Waraksa, L. Rudnicka, Application of micellar electrokinetic chromatography for detection of silver nanoparticles released from wound dressing, Electrophoresis 40 (2019) 1565–1572. https://doi.org/10.1002/elps.201900020.
[88] R. Singla, S. Soni, V. Patial, P.M. Kulurkar, A. Kumari, M. S., Y.S. Padwad, S.K. Yadav, In vivo diabetic wound healing potential of nanobiocomposites containing bamboo cellulose nanocrystals impregnated with silver nanoparticles, Int J Biol Macromol 105 (2017) 45–55. https://doi.org/10.1016/j.ijbiomac.2017.06.109.
[89] A.K. Chatterjee, R. Chakraborty, T. Basu, Mechanism of antibacterial activity of copper nanoparticles, Nanotechnology 25 (2014) 135101. https://doi.org/10.1088/0957-4484/25/13/135101.
[90] S. Alizadeh, B. Seyedalipour, S. Shafieyan, A. Kheime, P. Mohammadi, N. Aghdami, Copper nanoparticles promote rapid wound healing in acute full thickness defect via acceleration of skin cell migration, proliferation, and neovascularization, Biochem Biophys Res Commun 517 (2019) 684–690. https://doi.org/10.1016/j.bbrc.2019.07.110.
[91] S.M. Bauer, R.J. Bauer, O.C. Velazquez, Angiogenesis, Vasculogenesis, and Induction of Healing in Chronic Wounds, Vasc Endovascular Surg 39 (2005) 293–306. https://doi.org/10.1177/153857440503900401.
[92] Q. Li, F. Lu, G. Zhou, K. Yu, B. Lu, Y. Xiao, F. Dai, D. Wu, G. Lan, Silver Inlaid with Gold Nanoparticle/Chitosan Wound Dressing Enhances Antibacterial Activity and Porosity, and Promotes Wound Healing, Biomacromolecules 18 (2017) 3766–3775. https://doi.org/10.1021/acs.biomac.7b01180.
[93] M.H. Sarfraz, M. Zubair, B. Aslam, A. Ashraf, M.H. Siddique, S. Hayat, J.N. Cruz, S. Muzammil, M. Khurshid, M.F. Sarfraz, A. Hashem, T.M. Dawoud, G.D. Avila-Quezada, E.F. Abd_Allah, Comparative analysis of phyto-fabricated chitosan, copper oxide, and chitosan-based CuO nanoparticles: antibacterial potential against Acinetobacter baumannii isolates and anticancer activity against HepG2 cell lines, Front Microbiol 14 (2023). https://doi.org/10.3389/fmicb.2023.1188743.
[94] M.G. Arafa, R.F. El-Kased, M.M. Elmazar, Thermoresponsive gels containing gold nanoparticles as smart antibacterial and wound healing agents, Sci Rep 8 (2018) 13674. https://doi.org/10.1038/s41598-018-31895-4.
[95] P. Victor, D. Sarada, K.M. Ramkumar, Pharmacological activation of Nrf2 promotes wound healing, Eur J Pharmacol 886 (2020) 173395. https://doi.org/10.1016/j.ejphar.2020.173395.
[96] H. Kawaguchi, S. Jingushi, T. Izumi, M. Fukunaga, T. Matsushita, T. Nakamura, K. Mizuno, T. Nakamura, K. Nakamura, Local application of recombinant human fibroblast growth factor-2 on bone repair: A dose–escalation prospective trial on patients with osteotomy, Journal of Orthopaedic Research 25 (2007) 480–487. https://doi.org/10.1002/jor.20315.
[97] K.P. Hoversten, L.J. Kiemele, A.M. Stolp, P.Y. Takahashi, B.P. Verdoorn, Prevention, Diagnosis, and Management of Chronic Wounds in Older Adults, Mayo Clin Proc 95 (2020) 2021–2034. https://doi.org/10.1016/j.mayocp.2019.10.014.
[98] F.S. Alves, J.N. Cruz, I.N. de Farias Ramos, D.L. do Nascimento Brandão, R.N. Queiroz, G.V. da Silva, G.V. da Silva, M.F. Dolabela, M.L. da Costa, A.S. Khayat, J. de Arimatéia Rodrigues do Rego, D. do Socorro Barros Brasil, Evaluation of Antimicrobial Activity and Cytotoxicity Effects of Extracts of Piper nigrum L. and Piperine, Separations 10 (2023). https://doi.org/10.3390/separations10010021.
[99] P.D. Marcato, L.B. De Paula, P.S. Melo, I.R. Ferreira, A.B.A. Almeida, A.S. Torsoni, O.L. Alves, In Vivo Evaluation of Complex Biogenic Silver Nanoparticle and Enoxaparin in Wound Healing, J Nanomater 2015 (2015) 1–10. https://doi.org/10.1155/2015/439820.
[100] M.I.N. Ahamed, S. Sankar, P.M. Kashif, S.K.H. Basha, T.P. Sastry, Evaluation of biomaterial containing regenerated cellulose and chitosan incorporated with silver nanoparticles, Int J Biol Macromol 72 (2015) 680–686. https://doi.org/10.1016/j.ijbiomac.2014.08.055.
[101] X. Dai, Q. Guo, Y. Zhao, P. Zhang, T. Zhang, X. Zhang, C. Li, Functional Silver Nanoparticle as a Benign Antimicrobial Agent That Eradicates Antibiotic-Resistant Bacteria and Promotes Wound Healing, ACS Appl Mater Interfaces 8 (2016) 25798–25807. https://doi.org/10.1021/acsami.6b09267.
[102] M. Adibhesami, M. Ahmadi, A.A. Farshid, F. Sarrafzadeh-Rezaei, B. Dalir-Naghadeh, Effects of silver nanoparticles on Staphylococcus aureus contaminated open wounds healing in mice: An experimental study., Vet Res Forum 8 (2017) 23–28.
[103] C. You, Q. Li, X. Wang, P. Wu, J.K. Ho, R. Jin, L. Zhang, H. Shao, C. Han, Silver nanoparticle loaded collagen/chitosan scaffolds promote wound healing via regulating fibroblast migration and macrophage activation, Sci Rep 7 (2017) 10489. https://doi.org/10.1038/s41598-017-10481-0.
[104] H. Ye, J. Cheng, K. Yu, In situ reduction of silver nanoparticles by gelatin to obtain porous silver nanoparticle/chitosan composites with enhanced antimicrobial and wound-healing activity, Int J Biol Macromol 121 (2019) 633–642. https://doi.org/10.1016/j.ijbiomac.2018.10.056.
[105] F. Kong, C. Fan, Y. Yang, B.H. Lee, K. Wei, 5-hydroxymethylfurfural-embedded poly (vinyl alcohol)/sodium alginate hybrid hydrogels accelerate wound healing, Int J Biol Macromol 138 (2019) 933–949. https://doi.org/10.1016/j.ijbiomac.2019.07.152.
[106] V. Nagarjuna Reddy, S. Nyamathulla, K. Abdul Kadir Pahirulzaman, S.I. Mokhtar, N. Giribabu, V.R. Pasupuleti, Gallocatechin-silver nanoparticles embedded in cotton gauze patches accelerated wound healing in diabetic rats by promoting proliferation and inhibiting apoptosis through the Wnt/β-catenin signaling pathway, PLoS One 17 (2022) e0268505. https://doi.org/10.1371/journal.pone.0268505.
[107] W. Klinkajon, P. Supaphol, Novel copper (II) alginate hydrogels and their potential for use as anti-bacterial wound dressings, Biomedical Materials 9 (2014) 045008. https://doi.org/10.1088/1748-6041/9/4/045008.
[108] B. Tao, C. Lin, Y. Deng, Z. Yuan, X. Shen, M. Chen, Y. He, Z. Peng, Y. Hu, K. Cai, Copper-nanoparticle-embedded hydrogel for killing bacteria and promoting wound healing with photothermal therapy, J Mater Chem B 7 (2019) 2534–2548. https://doi.org/10.1039/C8TB03272F.
[109] Q. Xu, M. Chang, Y. Zhang, E. Wang, M. Xing, L. Gao, Z. Huan, F. Guo, J. Chang, PDA/Cu Bioactive Hydrogel with “Hot Ions Effect” for Inhibition of Drug-Resistant Bacteria and Enhancement of Infectious Skin Wound Healing, ACS Appl Mater Interfaces 12 (2020) 31255–31269. https://doi.org/10.1021/acsami.0c08890.
[110] Y. Yang, Z. Dong, M. Li, L. Liu, H. Luo, P. Wang, D. Zhang, X. Yang, K. Zhou, S. Lei,
Graphene Oxide/Copper Nanoderivatives-Modified Chitosan/Hyaluronic Acid Dressings for Facilitating Wound Healing in Infected Full-Thickness Skin Defects
, Int J Nanomedicine Volume 15 (2020) 8231–8247. https://doi.org/10.2147/IJN.S278631.
[111] E. Ghasemian Lemraski, H. Jahangirian, M. Dashti, E. Khajehali, Mis.S. Sharafinia, R. Rafiee-Moghaddam, T.J. Webster, Antimicrobial Double-Layer Wound Dressing Based on Chitosan/Polyvinyl Alcohol/Copper: In vitro and in vivo Assessment, Int J Nanomedicine Volume 16 (2021) 223–235. https://doi.org/10.2147/IJN.S266692.
[112] X. Sun, M. Dong, Z. Guo, H. Zhang, J. Wang, P. Jia, T. Bu, Y. Liu, L. Li, L. Wang, Multifunctional chitosan-copper-gallic acid based antibacterial nanocomposite wound dressing, Int J Biol Macromol 167 (2021) 10–22. https://doi.org/10.1016/j.ijbiomac.2020.11.153.
[113] B. Tao, C. Lin, A. Guo, Y. Yu, X. Qin, K. Li, H. Tian, W. Yi, D. Lei, L. Chen, Fabrication of copper ions-substituted hydroxyapatite/polydopamine nanocomposites with high antibacterial and angiogenesis effects for promoting infected wound healing, Journal of Industrial and Engineering Chemistry 104 (2021) 345–355. https://doi.org/10.1016/j.jiec.2021.08.035.
[114] M. Wang, A. Xia, S. Wu, J. Shen, Facile Synthesis of the Cu, N-CDs@GO-CS Hydrogel with Enhanced Antibacterial Activity for Effective Treatment of Wound Infection, Langmuir 37 (2021) 7928–7935. https://doi.org/10.1021/acs.langmuir.1c00529.
[115] H. Gu, P.L. Ho, E. Tong, L. Wang, B. Xu, Presenting Vancomycin on Nanoparticles to Enhance Antimicrobial Activities, Nano Lett 3 (2003) 1261–1263. https://doi.org/10.1021/nl034396z.
[116] S. Hsu, Y.-B. Chang, C.-L. Tsai, K.-Y. Fu, S.-H. Wang, H.-J. Tseng, Characterization and biocompatibility of chitosan nanocomposites, Colloids Surf B Biointerfaces 85 (2011) 198–206. https://doi.org/10.1016/j.colsurfb.2011.02.029.
[117] M.J. Cozad, S.L. Bachman, S.A. Grant, Assessment of decellularized porcine diaphragm conjugated with gold nanomaterials as a tissue scaffold for wound healing, J Biomed Mater Res A 99A (2011) 426–434. https://doi.org/10.1002/jbm.a.33182.
[118] Mohd.A. Sherwani, S. Tufail, A.A. Khan, M. Owais, Gold Nanoparticle-Photosensitizer Conjugate Based Photodynamic Inactivation of Biofilm Producing Cells: Potential for Treatment of C. albicans Infection in BALB/c Mice, PLoS One 10 (2015) e0131684. https://doi.org/10.1371/journal.pone.0131684.
[119] N. Volkova, M. Yukhta, O. Pavlovich, A. Goltsev, Application of Cryopreserved Fibroblast Culture with Au Nanoparticles to Treat Burns, Nanoscale Res Lett 11 (2016) 22. https://doi.org/10.1186/s11671-016-1242-y.
[120] O. Akturk, K. Kismet, A.C. Yasti, S. Kuru, M.E. Duymus, F. Kaya, M. Caydere, S. Hucumenoglu, D. Keskin, Collagen/gold nanoparticle nanocomposites: A potential skin wound healing biomaterial, J Biomater Appl 31 (2016) 283–301. https://doi.org/10.1177/0885328216644536.
[121] O. Akturk, K. Kismet, A.C. Yasti, S. Kuru, M.E. Duymus, F. Kaya, M. Caydere, S. Hucumenoglu, D. Keskin, Collagen/gold nanoparticle nanocomposites: A potential skin wound healing biomaterial, J Biomater Appl 31 (2016) 283–301. https://doi.org/10.1177/0885328216644536.
[122] Q. Li, F. Lu, G. Zhou, K. Yu, B. Lu, Y. Xiao, F. Dai, D. Wu, G. Lan, Silver Inlaid with Gold Nanoparticle/Chitosan Wound Dressing Enhances Antibacterial Activity and Porosity, and Promotes Wound Healing, Biomacromolecules 18 (2017) 3766–3775. https://doi.org/10.1021/acs.biomac.7b01180.
[123] A. Pan, M. Zhong, H. Wu, Y. Peng, H. Xia, Q. Tang, Q. Huang, L. Wei, L. Xiao, C. Peng, Topical Application of Keratinocyte Growth Factor Conjugated Gold Nanoparticles Accelerate Wound Healing, Nanomedicine 14 (2018) 1619–1628. https://doi.org/10.1016/j.nano.2018.04.007.
[124] N.N. Mahmoud, S. Hikmat, D. Abu Ghith, M. Hajeer, L. Hamadneh, D. Qattan, E.A. Khalil, Gold nanoparticles loaded into polymeric hydrogel for wound healing in rats: Effect of nanoparticles’ shape and surface modification, Int J Pharm 565 (2019) 174–186. https://doi.org/10.1016/j.ijpharm.2019.04.079.
[125] Y. Zou, R. Xie, E. Hu, P. Qian, B. Lu, G. Lan, F. Lu, Protein-reduced gold nanoparticles mixed with gentamicin sulfate and loaded into konjac/gelatin sponge heal wounds and kill drug-resistant bacteria, Int J Biol Macromol 148 (2020) 921–931. https://doi.org/10.1016/j.ijbiomac.2020.01.190.
[126] K. Wang, Z. Qi, S. Pan, S. Zheng, H. Wang, Y. Chang, H. Li, P. Xue, X. Yang, C. Fu, Preparation, characterization and evaluation of a new film based on chitosan, arginine and gold nanoparticle derivatives for wound-healing efficacy, RSC Adv 10 (2020) 20886–20899. https://doi.org/10.1039/D0RA03704D.
[127] P. Chen, L. Bian, X. Hu, Synergic Fabrication of Gold Nanoparticles Embedded Dextran/ Silk Sericin Nanomaterials for the Treatment and Care of Wound Healing, J Clust Sci 33 (2022) 2147–2156. https://doi.org/10.1007/s10876-021-02131-3.
[128] C. Xia, B. Ren, N. Liu, Y. Zheng, A Feasible Strategy of Fabricating of Gold-Encapsulated Dextran/Polyvinyl Alcohol Nanoparticles for the Treatment and Care of Wound Healing, J Clust Sci 33 (2022) 2179–2187. https://doi.org/10.1007/s10876-021-02132-2.
[129] S. Sharifi, M.J. Hajipour, L. Gould, M. Mahmoudi, Nanomedicine in Healing Chronic Wounds: Opportunities and Challenges, Mol Pharm 18 (2021) 550–575. https://doi.org/10.1021/acs.molpharmaceut.0c00346.
[130] L. Tang, J. Cheng, Nonporous silica nanoparticles for nanomedicine application, Nano Today 8 (2013) 290–312. https://doi.org/10.1016/j.nantod.2013.04.007.
[131] L. Chen, X. Zhou, C. He, Mesoporous silica nanoparticles for tissue‐engineering applications, WIREs Nanomedicine and Nanobiotechnology 11 (2019). https://doi.org/10.1002/wnan.1573.
[132] C.S. Yah, G.S. Simate, Nanoparticles as potential new generation broad spectrum antimicrobial agents, DARU Journal of Pharmaceutical Sciences 23 (2015) 43. https://doi.org/10.1186/s40199-015-0125-6.
[133] F. Menaa, A. Abdelghani, B. Menaa, Graphene nanomaterials as biocompatible and conductive scaffolds for stem cells: impact for tissue engineering and regenerative medicine, J Tissue Eng Regen Med 9 (2015) 1321–1338. https://doi.org/10.1002/term.1910.
[134] J. Zhou, X. Qi, Multi-walled carbon nanotubes/epilson-polylysine nanocomposite with enhanced antibacterial activity, Lett Appl Microbiol 52 (2011) 76–83. https://doi.org/10.1111/j.1472-765X.2010.02969.x.
[135] G.M. Neelgund, A. Oki, Z. Luo, Antimicrobial activity of CdS and Ag2S quantum dots immobilized on poly(amidoamine) grafted carbon nanotubes, Colloids Surf B Biointerfaces 100 (2012) 215–221. https://doi.org/10.1016/j.colsurfb.2012.05.012.
[136] F. Cui, J. Sun, J. Ji, X. Yang, K. Wei, H. Xu, Q. Gu, Y. Zhang, X. Sun, Carbon dots-releasing hydrogels with antibacterial activity, high biocompatibility, and fluorescence performance as candidate materials for wound healing, J Hazard Mater 406 (2021) 124330. https://doi.org/10.1016/j.jhazmat.2020.124330.
[137] S. Aslan, M. Deneufchatel, S. Hashmi, N. Li, L.D. Pfefferle, M. Elimelech, E. Pauthe, P.R. Van Tassel, Carbon nanotube-based antimicrobial biomaterials formed via layer-by-layer assembly with polypeptides, J Colloid Interface Sci 388 (2012) 268–273. https://doi.org/10.1016/j.jcis.2012.08.025.
[138] K.K. Patel, D.B. Surekha, M. Tripathi, Md.M. Anjum, M.S. Muthu, R. Tilak, A.K. Agrawal, S. Singh, Antibiofilm Potential of Silver Sulfadiazine-Loaded Nanoparticle Formulations: A Study on the Effect of DNase-I on Microbial Biofilm and Wound Healing Activity, Mol Pharm 16 (2019) 3916–3925. https://doi.org/10.1021/acs.molpharmaceut.9b00527.
[139] F. Saporito, G. Sandri, M.C. Bonferoni, S. Rossi, C. Boselli, A. Icaro Cornaglia, B. Mannucci, P. Grisoli, B. Vigani, F. Ferrari, Essential oil-loaded lipid nanoparticles for wound healing, Int J Nanomedicine Volume 13 (2017) 175–186. https://doi.org/10.2147/IJN.S152529.
[140] R.A.-B. Sanad, H.M. Abdel-Bar, Chitosan–hyaluronic acid composite sponge scaffold enriched with Andrographolide-loaded lipid nanoparticles for enhanced wound healing, Carbohydr Polym 173 (2017) 441–450. https://doi.org/10.1016/j.carbpol.2017.05.098.
[141] M. Fumakia, E.A. Ho, Nanoparticles Encapsulated with LL37 and Serpin A1 Promotes Wound Healing and Synergistically Enhances Antibacterial Activity, Mol Pharm 13 (2016) 2318–2331. https://doi.org/10.1021/acs.molpharmaceut.6b00099.
[142] A.B. Scriboni, V.M. Couto, L.N. de M. Ribeiro, I.A. Freires, F.C. Groppo, E. de Paula, M. Franz-Montan, K. Cogo-Müller, Fusogenic Liposomes Increase the Antimicrobial Activity of Vancomycin Against Staphylococcus aureus Biofilm, Front Pharmacol 10 (2019). https://doi.org/10.3389/fphar.2019.01401.
[143] Z. Rukavina, M. Šegvić Klarić, J. Filipović-Grčić, J. Lovrić, Ž. Vanić, Azithromycin-loaded liposomes for enhanced topical treatment of methicillin-resistant Staphyloccocus aureus (MRSA) infections, Int J Pharm 553 (2018) 109–119. https://doi.org/10.1016/j.ijpharm.2018.10.024.
[144] S. Wang, C. Yan, X. Zhang, D. Shi, L. Chi, G. Luo, J. Deng, Antimicrobial peptide modification enhances the gene delivery and bactericidal efficiency of gold nanoparticles for accelerating diabetic wound healing, Biomater Sci 6 (2018) 2757–2772. https://doi.org/10.1039/C8BM00807H.
[145] N. Monteiro, M. Martins, A. Martins, N.A. Fonseca, J.N. Moreira, R.L. Reis, N.M. Neves, Antibacterial activity of chitosan nanofiber meshes with liposomes immobilized releasing gentamicin, Acta Biomater 18 (2015) 196–205. https://doi.org/10.1016/j.actbio.2015.02.018.
[146] R.K. Thapa, K.L. Kiick, M.O. Sullivan, Encapsulation of collagen mimetic peptide-tethered vancomycin liposomes in collagen-based scaffolds for infection control in wounds, Acta Biomater 103 (2020) 115–128. https://doi.org/10.1016/j.actbio.2019.12.014.
[147] A. Kushwaha, L. Goswami, B.S. Kim, Nanomaterial-Based Therapy for Wound Healing, Nanomaterials 12 (2022) 618. https://doi.org/10.3390/nano12040618.
[148] M. Ramasamy, J. Lee, Recent Nanotechnology Approaches for Prevention and Treatment of Biofilm-Associated Infections on Medical Devices, Biomed Res Int 2016 (2016) 1–17. https://doi.org/10.1155/2016/1851242.
[149] Y.H. Ngo, D. Li, G.P. Simon, G. Garnier, Paper surfaces functionalized by nanoparticles, Adv Colloid Interface Sci 163 (2011) 23–38. https://doi.org/10.1016/j.cis.2011.01.004.
[150] T. Wang, Y. Zheng, Y. Shen, Y. Shi, F. Li, C. Su, L. Zhao, Chitosan nanoparticles loaded hydrogels promote skin wound healing through the modulation of reactive oxygen species, Artif Cells Nanomed Biotechnol 46 (2018) 138–149. https://doi.org/10.1080/21691401.2017.1415212.
[151] A. Ibrahim, H. Fatima, M.M. Babar, Targeted delivery of natural products, in: J.N. Cruz (Ed.), Drug Discovery and Design Using Natural Products, Springer Nature Switzerland, Cham, 2023: pp. 377–393. https://doi.org/10.1007/978-3-031-35205-8_12.
[152] H. Liu, C. Wang, C. Li, Y. Qin, Z. Wang, F. Yang, Z. Li, J. Wang, A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing, RSC Adv 8 (2018) 7533–7549. https://doi.org/10.1039/C7RA13510F.
[153] M.J. Mitchell, M.M. Billingsley, R.M. Haley, M.E. Wechsler, N.A. Peppas, R. Langer, Engineering precision nanoparticles for drug delivery, Nat Rev Drug Discov 20 (2021) 101–124. https://doi.org/10.1038/s41573-020-0090-8.
[154] R. Li, K. Liu, X. Huang, D. Li, J. Ding, B. Liu, X. Chen, Bioactive Materials Promote Wound Healing through Modulation of Cell Behaviors, Advanced Science 9 (2022). https://doi.org/10.1002/advs.202105152.
[155] S. Pina, J.M. Oliveira, R.L. Reis, Natural-Based Nanocomposites for Bone Tissue Engineering and Regenerative Medicine: A Review, Advanced Materials 27 (2015) 1143–1169. https://doi.org/10.1002/adma.201403354.
[156] F. Paladini, M. Pollini, Antimicrobial Silver Nanoparticles for Wound Healing Application: Progress and Future Trends, Materials 12 (2019) 2540. https://doi.org/10.3390/ma12162540.
[157] M. Ovais, I. Ahmad, A.T. Khalil, S. Mukherjee, R. Javed, M. Ayaz, A. Raza, Z.K. Shinwari, Wound healing applications of biogenic colloidal silver and gold nanoparticles: recent trends and future prospects, Appl Microbiol Biotechnol 102 (2018) 4305–4318. https://doi.org/10.1007/s00253-018-8939-z.
[158] G. Rath, T. Hussain, G. Chauhan, T. Garg, A.K. Goyal, Development and characterization of cefazolin loaded zinc oxide nanoparticles composite gelatin nanofiber mats for postoperative surgical wounds, Materials Science and Engineering: C 58 (2016) 242–253. https://doi.org/10.1016/j.msec.2015.08.050.
[159] F. Rezkita, K.G.P. Wibawa, A.P. Nugraha, Curcumin loaded Chitosan Nanoparticle for Accelerating the Post Extraction Wound Healing in Diabetes Mellitus Patient: A Review, Res J Pharm Technol 13 (2020) 1039. https://doi.org/10.5958/0974-360X.2020.00191.2.
[160] A. V Samrot, M.S. Sree, D. Rajalakshmi, L.N.R. Prakash, P. Prakash, Natural biopolymers as scaffold, in: J.N. Cruz (Ed.), Drug Discovery and Design Using Natural Products, Springer Nature Switzerland, Cham, 2023: pp. 23–36. https://doi.org/10.1007/978-3-031-35205-8_20.
[161] P. Dam, M. Celik, M. Ustun, S. Saha, C. Saha, E.A. Kacar, S. Kugu, E.N. Karagulle, S. Tasoglu, F. Buyukserin, R. Mondal, P. Roy, M.L.R. Macedo, O.L. Franco, M.H. Cardoso, S. Altuntas, A.K. Mandal, Wound healing strategies based on nanoparticles incorporated in hydrogel wound patches, RSC Adv 13 (2023) 21345–21364. https://doi.org/10.1039/D3RA03477A.
[162] S. Ahn, C.O. Chantre, A.R. Gannon, J.U. Lind, P.H. Campbell, T. Grevesse, B.B. O’Connor, K.K. Parker, Soy Protein/Cellulose Nanofiber Scaffolds Mimicking Skin Extracellular Matrix for Enhanced Wound Healing, Adv Healthc Mater 7 (2018) 1701175. https://doi.org/10.1002/adhm.201701175.
[163] R. Jangde, D. Singh, Preparation and optimization of quercetin-loaded liposomes for wound healing, using response surface methodology, Artif Cells Nanomed Biotechnol 44 (2016) 635–641. https://doi.org/10.3109/21691401.2014.975238.
[164] N. Hasan, J. Cao, J. Lee, S.P. Hlaing, M.A. Oshi, M. Naeem, M.-H. Ki, B.L. Lee, Y. Jung, J.-W. Yoo, Bacteria-Targeted Clindamycin Loaded Polymeric Nanoparticles: Effect of Surface Charge on Nanoparticle Adhesion to MRSA, Antibacterial Activity, and Wound Healing, Pharmaceutics 11 (2019) 236. https://doi.org/10.3390/pharmaceutics11050236.
[165] P. Dam, M. Celik, M. Ustun, S. Saha, C. Saha, E.A. Kacar, S. Kugu, E.N. Karagulle, S. Tasoglu, F. Buyukserin, R. Mondal, P. Roy, M.L.R. Macedo, O.L. Franco, M.H. Cardoso, S. Altuntas, A.K. Mandal, Wound healing strategies based on nanoparticles incorporated in hydrogel wound patches, RSC Adv 13 (2023) 21345–21364. https://doi.org/10.1039/D3RA03477A.
[166] J. Wu, M.D. Weir, M.A.S. Melo, H.H.K. Xu, Development of novel self-healing and antibacterial dental composite containing calcium phosphate nanoparticles, J Dent 43 (2015) 317–326. https://doi.org/10.1016/j.jdent.2015.01.009.
[167] Y. Liang, X. Zhao, T. Hu, Y. Han, B. Guo, Mussel-inspired, antibacterial, conductive, antioxidant, injectable composite hydrogel wound dressing to promote the regeneration of infected skin, J Colloid Interface Sci 556 (2019) 514–528. https://doi.org/10.1016/j.jcis.2019.08.083.
[168] J. Anjana, V.K. Rajan, R. Biswas, R. Jayakumar, Controlled Delivery of Bioactive Molecules for the Treatment of Chronic Wounds, Curr Pharm Des 23 (2017). https://doi.org/10.2174/1381612823666170503145528.
[169] K. Rahim, S. Saleha, X. Zhu, L. Huo, A. Basit, O.L. Franco, Bacterial Contribution in Chronicity of Wounds, Microb Ecol 73 (2017) 710–721. https://doi.org/10.1007/s00248-016-0867-9.
[170] M.A. Pérez-Díaz, L. Boegli, G. James, C. Velasquillo, R. Sánchez-Sánchez, R.-E. Martínez-Martínez, G.A. Martínez-Castañón, F. Martinez-Gutierrez, Silver nanoparticles with antimicrobial activities against Streptococcus mutans and their cytotoxic effect, Materials Science and Engineering: C 55 (2015) 360–366. https://doi.org/10.1016/j.msec.2015.05.036.
[171] A.J. Kora, R.B. Sashidhar, Antibacterial activity of biogenic silver nanoparticles synthesized with gum ghatti and gum olibanum: a comparative study, J Antibiot (Tokyo) 68 (2015) 88–97. https://doi.org/10.1038/ja.2014.114.
[172] M. Stevanović, Kovačević, Petković, Filipič, Uskoković, Effect of poly-α, γ, L-glutamic acid as a capping agent on morphology and oxidative stress-dependent toxicity of silver nanoparticles, Int J Nanomedicine (2011) 2837. https://doi.org/10.2147/IJN.S24889.
[173] N.J. Amruthraj, J.P. Preetam Raj, A. Lebel, Capsaicin-capped silver nanoparticles: its kinetics, characterization and biocompatibility assay, Appl Nanosci 5 (2015) 403–409. https://doi.org/10.1007/s13204-014-0330-5.
[174] S.K. Nethi, A.K. Barui, S. Mukherjee, C.R. Patra, Engineered Nanoparticles for Effective Redox Signaling During Angiogenic and Antiangiogenic Therapy, Antioxid Redox Signal 30 (2019) 786–809. https://doi.org/10.1089/ars.2017.7383.
[175] K.P. Claffey, L.F. Brown, L.F. del Aguila, K. Tognazzi, K.T. Yeo, E.J. Manseau, H.F. Dvorak, Expression of vascular permeability factor/vascular endothelial growth factor by melanoma cells increases tumor growth, angiogenesis, and experimental metastasis., Cancer Res 56 (1996) 172–81.
[176] H. Xu, F. Lv, Y. Zhang, Z. Yi, Q. Ke, C. Wu, M. Liu, J. Chang, Hierarchically micro-patterned nanofibrous scaffolds with a nanosized bio-glass surface for accelerating wound healing, Nanoscale 7 (2015) 18446–18452. https://doi.org/10.1039/C5NR04802H.
[177] Y. Zhang, M. Chang, F. Bao, M. Xing, E. Wang, Q. Xu, Z. Huan, F. Guo, J. Chang, Multifunctional Zn doped hollow mesoporous silica/polycaprolactone electrospun membranes with enhanced hair follicle regeneration and antibacterial activity for wound healing, Nanoscale 11 (2019) 6315–6333. https://doi.org/10.1039/C8NR09818B.
[178] S.-C. Tao, B.-Y. Rui, Q.-Y. Wang, D. Zhou, Y. Zhang, S.-C. Guo, Extracellular vesicle-mimetic nanovesicles transport LncRNA-H19 as competing endogenous RNA for the treatment of diabetic wounds, Drug Deliv 25 (2018) 241–255. https://doi.org/10.1080/10717544.2018.1425774.
[179] S. Chigurupati, M.R. Mughal, E. Okun, S. Das, A. Kumar, M. McCaffery, S. Seal, M.P. Mattson, Effects of cerium oxide nanoparticles on the growth of keratinocytes, fibroblasts and vascular endothelial cells in cutaneous wound healing, Biomaterials 34 (2013) 2194–2201. https://doi.org/10.1016/j.biomaterials.2012.11.061.
[180] J.E. Kim, J. Lee, M. Jang, M.H. Kwak, J. Go, E.K. Kho, S.H. Song, J.E. Sung, J. Lee, D.Y. Hwang, Accelerated healing of cutaneous wounds using phytochemically stabilized gold nanoparticle deposited hydrocolloid membranes, Biomater Sci 3 (2015) 509–519. https://doi.org/10.1039/C4BM00390J.
[181] P. Lau, N. Bidin, S. Islam, W.N.B.W.M. Shukri, N. Zakaria, N. Musa, G. Krishnan, Influence of gold nanoparticles on wound healing treatment in rat model: Photobiomodulation therapy, Lasers Surg Med 49 (2017) 380–386. https://doi.org/10.1002/lsm.22614.
[182] R.H. Adams, A. Eichmann, Axon Guidance Molecules in Vascular Patterning, Cold Spring Harb Perspect Biol 2 (2010) a001875–a001875. https://doi.org/10.1101/cshperspect.a001875.
[183] J. Yang, The role of reactive oxygen species in angiogenesis and preventing tissue injury after brain ischemia, Microvasc Res 123 (2019) 62–67. https://doi.org/10.1016/j.mvr.2018.12.005.
[184] S.Y. Wang, H. Kim, G. Kwak, H.Y. Yoon, S.D. Jo, J.E. Lee, D. Cho, I.C. Kwon, S.H. Kim, Development of Biocompatible HA Hydrogels Embedded with a New Synthetic Peptide Promoting Cellular Migration for Advanced Wound Care Management, Advanced Science 5 (2018) 1800852. https://doi.org/10.1002/advs.201800852.
[185] D. Zhao, M. Liu, Q. Li, X. Zhang, C. Xue, Y. Lin, X. Cai, Tetrahedral DNA Nanostructure Promotes Endothelial Cell Proliferation, Migration, and Angiogenesis via Notch Signaling Pathway, ACS Appl Mater Interfaces 10 (2018) 37911–37918. https://doi.org/10.1021/acsami.8b16518.
[186] S. Schoors, U. Bruning, R. Missiaen, K.C.S. Queiroz, G. Borgers, I. Elia, A. Zecchin, A.R. Cantelmo, S. Christen, J. Goveia, W. Heggermont, L. Goddé, S. Vinckier, P.P. Van Veldhoven, G. Eelen, L. Schoonjans, H. Gerhardt, M. Dewerchin, M. Baes, K. De Bock, B. Ghesquière, S.Y. Lunt, S.-M. Fendt, P. Carmeliet, Fatty acid carbon is essential for dNTP synthesis in endothelial cells, Nature 520 (2015) 192–197. https://doi.org/10.1038/nature14362.
[187] J.E. Kim, J. Lee, M. Jang, M.H. Kwak, J. Go, E.K. Kho, S.H. Song, J.E. Sung, J. Lee, D.Y. Hwang, Accelerated healing of cutaneous wounds using phytochemically stabilized gold nanoparticle deposited hydrocolloid membranes, Biomater Sci 3 (2015) 509–519. https://doi.org/10.1039/C4BM00390J.
[188] P. Lau, N. Bidin, S. Islam, W.N.B.W.M. Shukri, N. Zakaria, N. Musa, G. Krishnan, Influence of gold nanoparticles on wound healing treatment in rat model: Photobiomodulation therapy, Lasers Surg Med 49 (2017) 380–386. https://doi.org/10.1002/lsm.22614.
[189] W.-Y. Chen, H.-Y. Chang, J.-K. Lu, Y.-C. Huang, S.G. Harroun, Y.-T. Tseng, Y.-J. Li, C.-C. Huang, H.-T. Chang, Self-Assembly of Antimicrobial Peptides on Gold Nanodots: Against Multidrug-Resistant Bacteria and Wound-Healing Application, Adv Funct Mater 25 (2015) 7189–7199. https://doi.org/10.1002/adfm.201503248.
[190] F. Öri, R. Dietrich, C. Ganz, M. Dau, D. Wolter, A. Kasten, T. Gerber, B. Frerich, Silicon-dioxide−polyvinylpyrrolidone as a wound dressing for skin defects in a murine model, Journal of Cranio-Maxillofacial Surgery 45 (2017) 99–107. https://doi.org/10.1016/j.jcms.2016.10.002.
[191] X. Wang, F. Lv, T. Li, Y. Han, Z. Yi, M. Liu, J. Chang, C. Wu, Electrospun Micropatterned Nanocomposites Incorporated with Cu 2 S Nanoflowers for Skin Tumor Therapy and Wound Healing, ACS Nano 11 (2017) 11337–11349. https://doi.org/10.1021/acsnano.7b05858.
[192] Y. Xiao, D. Xu, H. Song, F. Shu, P. Wei, X. Yang, C. Zhong, X. Wang, W.E. Müller, Y. Zheng, S. Xiao, Z. Xia,
Cuprous oxide nanoparticles reduces hypertrophic scarring by inducing fibroblast apoptosis
, Int J Nanomedicine Volume 14 (2019) 5989–6000. https://doi.org/10.2147/IJN.S196794.
[193] S.K. Nethi, A.K. Barui, V.S. Bollu, B.R. Rao, C.R. Patra, Pro-angiogenic Properties of Terbium Hydroxide Nanorods: Molecular Mechanisms and Therapeutic Applications in Wound Healing, ACS Biomater Sci Eng 3 (2017) 3635–3645. https://doi.org/10.1021/acsbiomaterials.7b00457.
[194] M. Shi, L. Xia, Z. Chen, F. Lv, H. Zhu, F. Wei, S. Han, J. Chang, Y. Xiao, C. Wu, Europium-doped mesoporous silica nanosphere as an immune-modulating osteogenesis/angiogenesis agent, Biomaterials 144 (2017) 176–187. https://doi.org/10.1016/j.biomaterials.2017.08.027.
[195] A.K. Barui, S.K. Nethi, S. Haque, P. Basuthakur, C.R. Patra, Recent Development of Metal Nanoparticles for Angiogenesis Study and Their Therapeutic Applications, ACS Appl Bio Mater 2 (2019) 5492–5511. https://doi.org/10.1021/acsabm.9b00587.
[196] D. Hao, G. Zhang, Y. Gong, Z. Ma, Development and biological evaluation of cerium oxide loaded polycaprolactone dressing on cutaneous wound healing in nursing care, Mater Lett 265 (2020) 127401. https://doi.org/10.1016/j.matlet.2020.127401.
[197] S.M. Carvalho, C.D.F. Moreira, A.C.X. Oliveira, A.A.R. Oliveira, E.M.F. Lemos, M.M. Pereira, Bioactive glass nanoparticles for periodontal regeneration and applications in dentistry, in: Nanobiomaterials in Clinical Dentistry, Elsevier, 2019: pp. 351–383. https://doi.org/10.1016/B978-0-12-815886-9.00015-2.
[198] K. Varaprasad, Co-assembled ZnO (shell) – CuO (core) nano-oxide materials for microbial protection, Phosphorus Sulfur Silicon Relat Elem 193 (2018) 74–80. https://doi.org/10.1080/10426507.2017.1417301.
[199] S. Varshney, A. Nigam, S.J. Pawar, N. Mishra, An overview on biomedical applications of versatile silica nanoparticles, synthesized via several chemical and biological routes: A review, Phosphorus Sulfur Silicon Relat Elem 197 (2022) 72–88. https://doi.org/10.1080/10426507.2021.2017434.
[200] M. Sharifiaghdam, E. Shaabani, F. Asghari, R. Faridi‐Majidi, Chitosan coated metallic nanoparticles with stability, antioxidant, and antibacterial properties: Potential for wound healing application, J Appl Polym Sci 139 (2022). https://doi.org/10.1002/app.51766.
[201] P. Deng, X. Liang, F. Chen, Y. Chen, J. Zhou, Novel multifunctional dual-dynamic-bonds crosslinked hydrogels for multi-strategy therapy of MRSA-infected wounds, Appl Mater Today 26 (2022) 101362. https://doi.org/10.1016/j.apmt.2022.101362.
[202] K. Zhang, G. Zhao, An Effective Wound Healing Material Based on Gold Incorporation into a Heparin-Polyvinyl Alcohol Nanocomposite: Enhanced In Vitro and In Vivo Care of Perioperative Period, J Clust Sci 33 (2022) 1655–1665. https://doi.org/10.1007/s10876-021-02078-5.
[203] E. Ghasemian Lemraski, H. Jahangirian, M. Dashti, E. Khajehali, Mis.S. Sharafinia, R. Rafiee-Moghaddam, T.J. Webster, Antimicrobial Double-Layer Wound Dressing Based on Chitosan/Polyvinyl Alcohol/Copper: In vitro and in vivo Assessment, Int J Nanomedicine Volume 16 (2021) 223–235. https://doi.org/10.2147/IJN.S266692.
[204] M. Bandeira, B.S. Chee, R. Frassini, M. Nugent, M. Giovanela, M. Roesch-Ely, J. da S. Crespo, D.M. Devine, Antimicrobial PAA/PAH Electrospun Fiber Containing Green Synthesized Zinc Oxide Nanoparticles for Wound Healing, Materials 14 (2021) 2889. https://doi.org/10.3390/ma14112889.
[205] V.A.T. Le, T.X. Trinh, P.N. Chien, N.N. Giang, X.-R. Zhang, S.-Y. Nam, C.-Y. Heo, Evaluation of the Performance of a ZnO-Nanoparticle-Coated Hydrocolloid Patch in Wound Healing, Polymers (Basel) 14 (2022) 919. https://doi.org/10.3390/polym14050919.
[206] A. Sathiyaseelan, K. Saravanakumar, A.V.A. Mariadoss, M.-H. Wang, Antimicrobial and Wound Healing Properties of FeO Fabricated Chitosan/PVA Nanocomposite Sponge, Antibiotics 10 (2021) 524. https://doi.org/10.3390/antibiotics10050524.
[207] K. Zamani, N. Allah-Bakhshi, F. Akhavan, M. Yousefi, R. Golmoradi, M. Ramezani, H. Bach, S. Razavi, G.-R. Irajian, M. Gerami, A. Pakdin-Parizi, M. Tafrihi, F. Ramezani, Antibacterial effect of cerium oxide nanoparticle against Pseudomonas aeruginosa, BMC Biotechnol 21 (2021) 68. https://doi.org/10.1186/s12896-021-00727-1.
[208] Y. Lv, Y. Xu, X. Sang, C. Li, Y. Liu, Q. Guo, S. Ramakrishna, C. Wang, P. Hu, H.S. Nanda, PLLA–gelatin composite fiber membranes incorporated with functionalized CeNPs as a sustainable wound dressing substitute promoting skin regeneration and scar remodeling, J Mater Chem B 10 (2022) 1116–1127. https://doi.org/10.1039/D1TB02677A.
[209] M.E. David, R.M. Ion, R.M. Grigorescu, L. Iancu, A.M. Holban, F. Iordache, A.I. Nicoara, E. Alexandrescu, R. Somoghi, S. Teodorescu, A.I. Gheboianu, Biocompatible and Antimicrobial Cellulose Acetate-Collagen Films Containing MWCNTs Decorated with TiO2 Nanoparticles for Potential Biomedical Applications, Nanomaterials 12 (2022) 239. https://doi.org/10.3390/nano12020239.
[210] S.K. Karuppannan, R. Ramalingam, S.B. Mohamed Khalith, S.A. Musthafa, M.J.H. Dowlath, G. Munuswamy-Ramanujam, K.D. Arunachalam, Copper oxide nanoparticles infused electrospun polycaprolactone/gelatin scaffold as an antibacterial wound dressing, Mater Lett 294 (2021) 129787. https://doi.org/10.1016/j.matlet.2021.129787.
[211] I. Kalashnikova, S. Das, S. Seal, Nanomaterials for wound healing: scope and advancement, Nanomedicine 10 (2015) 2593–2612. https://doi.org/10.2217/nnm.15.82.
[212] P. Sundaram, H. Abrahamse, Phototherapy Combined with Carbon Nanomaterials (1D and 2D) and Their Applications in Cancer Therapy, Materials 13 (2020) 4830. https://doi.org/10.3390/ma13214830.
[213] S. Gurunathan, J. Woong Han, A. Abdal Daye, V. Eppakayala, J. Kim, Oxidative stress-mediated antibacterial activity of graphene oxide and reduced graphene oxide in Pseudomonas aeruginosa, Int J Nanomedicine (2012) 5901. https://doi.org/10.2147/IJN.S37397.
[214] H. Fatima, A. Ibrahim, S.D.A. Hamdani, T.A. Rajput, A. Noor, A. Gul, M.M. Babar, Natural product formulations to overcome poor ADMET properties, in: J.N. Cruz (Ed.), Drug Discovery and Design Using Natural Products, Springer Nature Switzerland, Cham, 2023: pp. 435–452. https://doi.org/10.1007/978-3-031-35205-8_15.
[215] Y. Zheng, S. Li, D. Han, L. Kong, J. Wang, M. Zhao, W. Cheng, H. Ju, Z. Yang, S. Ding, Eco-Friendly Preparation of Epoxy-Rich Graphene Oxide for Wound Healing, ACS Biomater Sci Eng 7 (2021) 752–763. https://doi.org/10.1021/acsbiomaterials.0c01598.
[216] B. Lu, T. Li, H. Zhao, X. Li, C. Gao, S. Zhang, E. Xie, Graphene-based composite materials beneficial to wound healing, Nanoscale 4 (2012) 2978. https://doi.org/10.1039/c2nr11958g.
[217] K. Banihashemi, N. Amirmozafari, I. Mehregan, R. Bakhtiari, B. Sobouti, Antibacterial effect of carbon nanotube containing chemical compounds on drug-resistant isolates of Acinetobacter baumannii, Iran J Microbiol (2021). https://doi.org/10.18502/ijm.v13i1.5501.
[218] B. Lu, T. Li, H. Zhao, X. Li, C. Gao, S. Zhang, E. Xie, Graphene-based composite materials beneficial to wound healing, Nanoscale 4 (2012) 2978. https://doi.org/10.1039/c2nr11958g.
[219] A.J. Monteforte, B. Lam, S. Das, S. Mukhopadhyay, C.S. Wright, P.E. Martin, A.K. Dunn, A.B. Baker, Glypican-1 nanoliposomes for potentiating growth factor activity in therapeutic angiogenesis, Biomaterials 94 (2016) 45–56. https://doi.org/10.1016/j.biomaterials.2016.03.048.
[220] K.K. Chereddy, C.-H. Her, M. Comune, C. Moia, A. Lopes, P.E. Porporato, J. Vanacker, M.C. Lam, L. Steinstraesser, P. Sonveaux, H. Zhu, L.S. Ferreira, G. Vandermeulen, V. Préat, PLGA nanoparticles loaded with host defense peptide LL37 promote wound healing, Journal of Controlled Release 194 (2014) 138–147. https://doi.org/10.1016/j.jconrel.2014.08.016.
[221] K. Han, K.-D. Lee, Z.-G. Gao, J.-S. Park, Preparation and evaluation of poly(l-lactic acid) microspheres containing rhEGF for chronic gastric ulcer healing, Journal of Controlled Release 75 (2001) 259–269. https://doi.org/10.1016/S0168-3659(01)00400-X.
[222] A. Schwentker, Y. Vodovotz, R. Weller, T.R. Billiar, Nitric oxide and wound repair: role of cytokines?, Nitric Oxide 7 (2002) 1–10. https://doi.org/10.1016/S1089-8603(02)00002-2.
[223] S. Chen, B. Liu, M.A. Carlson, A.F. Gombart, D.A. Reilly, J. Xie, Recent advances in electrospun nanofibers for wound healing, Nanomedicine 12 (2017) 1335–1352. https://doi.org/10.2217/nnm-2017-0017.
[224] W. Cheng, R. Xu, D. Li, C. Bortolini, J. He, M. Dong, F. Besenbacher, Y. Huang, M. Chen, Artificial extracellular matrix delivers TGFb1 regulating myofibroblast differentiation, RSC Adv 6 (2016) 21922–21928. https://doi.org/10.1039/C5RA26164C.
[225] J.E. Martín-Alfonso, A.A. Cuadri, M. Berta, M. Stading, Relation between concentration and shear-extensional rheology properties of xanthan and guar gum solutions, Carbohydr Polym 181 (2018) 63–70. https://doi.org/10.1016/j.carbpol.2017.10.057.
[226] L.A. De Louise, Morphology-Dependent Titanium Dioxide Nanoparticle-Induced Keratinocyte Toxicity And Exacerbation Of Allergic Contact Dermatitis, Toxicology: Current Research 4 (2020) 1–7. https://doi.org/10.24966/TCR-3735/100019.
[227] X. Lai, M. Wang, Y. Zhu, X. Feng, H. Liang, J. Wu, L. Nie, L. Li, L. Shao, ZnO NPs delay the recovery of psoriasis-like skin lesions through promoting nuclear translocation of p-NFκB p65 and cysteine deficiency in keratinocytes, J Hazard Mater 410 (2021) 124566. https://doi.org/10.1016/j.jhazmat.2020.124566.
[228] S. Hashempour, S. Ghanbarzadeh, H.I. Maibach, M. Ghorbani, H. Hamishehkar, Skin toxicity of topically applied nanoparticles, Ther Deliv 10 (2019) 383–396. https://doi.org/10.4155/tde-2018-0060.
[229] K. Sooklert, S. Nilyai, R. Rojanathanes, D. Jindatip, N. Sae-liang, N. Kitkumthorn, A. Mutirangura, A. Sereemaspun,
N-acetylcysteine reverses the decrease of DNA methylation status caused by engineered gold, silicon, and chitosan nanoparticles
, Int J Nanomedicine Volume 14 (2019) 4573–4587. https://doi.org/10.2147/IJN.S204372.
[230] M.S. Bakshi, Nanotoxicity in Systemic Circulation and Wound Healing, Chem Res Toxicol 30 (2017) 1253–1274. https://doi.org/10.1021/acs.chemrestox.7b00068.
[231] N. Hadrup, A.K. Sharma, K. Loeschner, Toxicity of silver ions, metallic silver, and silver nanoparticle materials after in vivo dermal and mucosal surface exposure: A review, Regulatory Toxicology and Pharmacology 98 (2018) 257–267. https://doi.org/10.1016/j.yrtph.2018.08.007.