Nano Antibiotics: Prospects and Challenges
V.P. Jayachandran
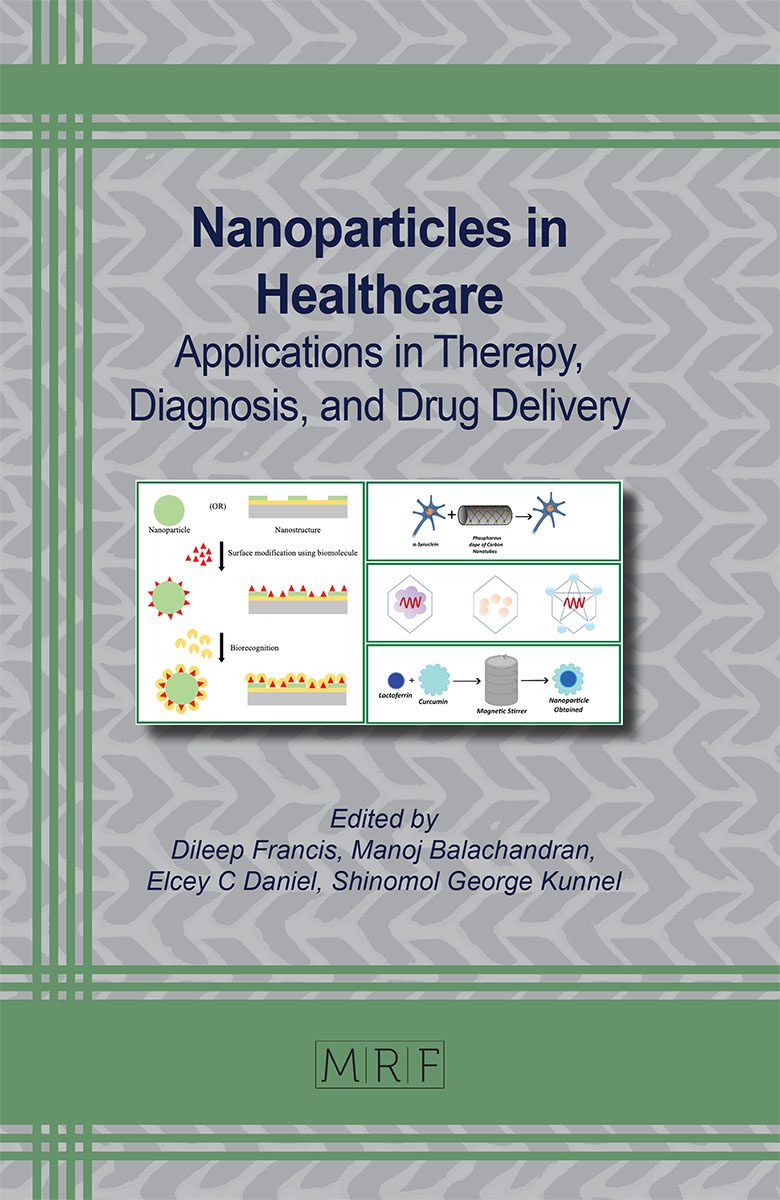
Antibiotic resistance is a major global public health concern, resulting in high healthcare costs, increased morbidity, and mortality. With a limited number of new antibiotics being developed, the emergence and spread of antibacterial resistance poses a constant threat to public health. After 1980s the antibiotic pipeline began to dry up and fewer new drugs were introduced, and microbes seem to be on the winning side in tiding over the barricades built by drugs. Adoption of an effective strategy to intervene the burning issue of MDR is a necessity of the hour. Nanotechnology gives great hope to the medical community in their fight against pathogens. As an essential byproduct nanoantibiotics (nAbts) are being developed by conjugating nanoparticles with antibiotic molecules. Various types of nanoparticles are used as drug delivery systems. This chapter explores the prospects of nAbts, the composition and types of nAbts, their mode of action, challenges faced by nAbts in terms of safety, toxicity, manufacturing complexity, regulatory hurdles etc. as well as development of resistance among bacterial pathogens against nAbts.
Keywords
Multidrug Resistance, Nano Antibiotics, Drug Delivery, Biocompatible, Liposome
Published online 2/10/2024, 30 pages
Citation: V.P. Jayachandran, Nano Antibiotics: Prospects and Challenges, Materials Research Foundations, Vol. 160, pp 83-112, 2024
DOI: https://doi.org/10.21741/9781644902974-4
Part of the book on Nanoparticles in Healthcare
References
[1] Information on (https://www.who.int/mediacentre/factsheets
[2] Information on (https://www.who.int/world-health-day/2011).
[3] Kamini, W. (2006). Emerging Problem of Antimicrobial Resistance in Developing Countries: Interwining Socioeconomic Issues. Regional Health Forum WHO South-East Asia Region, 7, [8-12].
[4] Nikaido, H. (2009). Multidrug Resistance in Bacteria. Annual Review of Biochemistry, 78(1), [119-146]. doi: 10.1146/annurev.biochem.78.082907.145923
[5] Laxminarayan, R., Matsoso, P., Pant, S., Brower, C., Røttingen, J.-A., Klugman, K., et al. (2016). Access to Effective Antimicrobials: A Worldwide Challenge. The Lancet, 387(10014), [168-175]. doi: 10.1016/S0140-6736(15)00474-2
[6] Christopher, J. L. M., Kevin S I., Fablina, S et al., Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet (2022) 399(10325) P[629-655], https://doi.org/10.1016/S0140-6736(21)02724-0
[7] Ventola, C. L. (2015). The antibiotic resistance crisis: Part 1: Causes and threats. P&T, 40(4), [277-283]. PMID: 25859123; PMCID: PMC4378521.
[8] Spellberg, B., & Gilbert, D. N. (2014). The future of antibiotics and resistance: A tribute to a career of leadership by John Bartlett. Clinical Infectious Diseases, 59(Suppl 2), S71-S75. https://doi.org/10.1093/cid/ciu392
[9] Freestone, I., Nigel, M., Margaret, Sax., Catherine, Higgitt.,(2007) The Lycurgus Cup-A Roman Nanotechnology.2007. Gold Bulletin 40(4):[270-277] DOI:10.1007/BF03215599
[10] Information on https://www.azonano.com/
[11] Soares, S., Sousa, J., Pais, A., & Vitorino, C. (2018). Nanomedicine: Principles, Properties, and Regulatory Issues. Frontiers in Chemistry, 6. doi: 10.3389/fchem.2018.0036
[12] Mamun, M. M., Sorinolu, A. J., Munir, M., & Vejerano, E. P. (2021). Nanoantibiotics: Functions and Properties at the Nanoscale to Combat Antibiotic Resistance. Frontiers in Chemistry, 9, 687660. doi: 10.3389/fchem.2021.687660
[13] Huh, A. J., & Kwon, Y. J. (2011). “Nanoantibiotics”: A new paradigm for treating infectious diseases using nanomaterials in the antibiotics resistant era. Journal of Controlled Release, 156(2), [128-145]. doi: 10.1016/j.jconrel.2011.07.002
[14] Jiang, Y., Zheng, W., Tran, K., et al. (2022). Hydrophilic nanoparticles that kill bacteria while sparing mammalian cells reveal the antibiotic role of nanostructures. Nature Communications, 13, 197. https://doi.org/10.1038/s41467-021-27193-9
[15] Ana Isabel Ribeiro, Alice Maria Dias, and Andrea Zille. (2022). Synergistic Effects Between Metal Nanoparticles and Commercial Antimicrobial Agents: A Review. ACS Appl. Nano Mater., 5, [3030-3064]. https://doi.org/10.1021/acsanm.1c03891
[16] Kotrange, H., Najda, A., Bains, A., Gruszecki, R., Chawla, P., Tosif M. M.( 2021). Metal and Metal Oxide Nanoparticle as a Novel Antibiotic Carrier for the Direct Delivery of Antibiotics. Int J Mol Sci. 4;22(17):9596. doi: 10.3390/ijms22179596.
[17] Neouze, M.-A., & Schubert, U. (2008). Surface Modification and Functionalization of Metal and Metal Oxide Nanoparticles by Organic Ligands. Monatshefte für Chemie – Chemical Monthly, 139(3), [183-195]. https://doi.org/10.1007/s00706-007-0775-2
[18] Payne, J. N., Waghwani, H. K., Connor, M. G., et al. (2016). Novel Synthesis of Kanamycin Conjugated Gold Nanoparticles with Potent Antibacterial Activity. Front Microbiol., 7, 607. doi: 10.3389/fmicb.2016.00607.
[19] Patil, T., Khot, V., & Pandey-Tiwari, A. (2022). Single-step antibiotic-mediated synthesis of kanamycin-conjugated gold nanoparticles for broad-spectrum antibacterial applications. Lett Appl Microbiol., 75(4), [913-923]. doi: 10.1111/lam.13764. PMID: 35689349.
[20] Armijo, L. M., Wawrzyniec, S. J., Kopciuch, M., Brandt, Y. I., Rivera, A. C., Withers, N. J., et al. (2020). Antibacterial Activity of Iron Oxide, Iron Nitride, and Tobramycin Conjugated Nanoparticles against Pseudomonas Aeruginosa Biofilms. Journal of Nanobiotechnology, 18(1), 35. doi: 10.1186/s12951-020-0588-6
[21] Carver, J. A., Simpson, A. L., Rathi, R. P., Normil, N., Lee, A. G., Force, M. D., et al. (2020). Functionalized Single-Walled Carbon Nanotubes and Nanographene Oxide to Overcome Antibiotic Resistance in Tetracycline-Resistant Escherichia Coli. ACS Applied Nano Materials, 3(4), [3910-3921]. doi: 10.1021/acsanm.0c00677
[22] van Dongen, M. A., Silpe, J. E., Dougherty, C. A., Kanduluru, A. K., Choi, S. K., Orr, B. G., Low, P. S., & Banaszak Holl, M. M. (2014). Avidity mechanism of dendrimer-folic acid conjugates. Molecular Pharmaceutics, 11, [1696-1706]. doi: 10.1021/mp5000967
[23] Falanga, A., Del Genio, V., & Galdiero, S. (2021). Peptides and dendrimers: How to combat viral and bacterial infections. Pharmaceutics, 13(1), 101. doi: 10.3390/pharmaceutics13010101
[24] Chis, A. A., Dobrea, C., Morgovan, C., & Bălşeanu, T. A. (2020). Applications and limitations of dendrimers in biomedicine. Molecules, 25(17), 3982. doi: 10.3390/molecules25173982
[25] Kannan, R. M., Nance, E., Kannan, S., & Tomalia, D. A. (2014). Emerging concepts in dendrimer-based nanomedicine: From design principles to clinical applications. Journal of Internal Medicine, 276, [579-617]. doi: 10.1111/joim.12280.
[26] Wu, Z. L., Zhao, J., & Xu, R. (2020). Recent Advances in Oral Nano-Antibiotics for Bacterial Infection Therapy. International Journal of Nanomedicine, 15, 9587-9610. https://doi.org/10.2147/IJN.S279652
[27] Lopes-de-Campos, D., Pinto, R. M., Lima, S. A. C., et al. (2019). Delivering amoxicillin at the infection site – a rational design through lipid nanoparticles. International Journal of Nanomedicine, 14, [2781-2795]. https://doi.org/10.2147/IJN.S193135
[28] Kazeminava, F., Javanbakht, S., Nouri, M., Gholamzadeh, P., Rajabnia, R., & Mohammadi-Samani, S. (2022). Gentamicin-loaded chitosan/folic acid-based carbon quantum dots nanocomposite hydrogel films as potential antimicrobial wound dressing. Journal of Biological Engineering, 16(1), 36. doi: 10.1186/s13036-022-00318-4.
[29] Razei, A., Cheraghali, A. M., Saadati, M., Khosravi, A. D., & Lotfi, M. (2019). Gentamicin-loaded chitosan nanoparticles improve its therapeutic effects on Brucella-infected J774A.1 murine cells. Galen Medical Journal, 8, e1296. doi: 10.31661/gmj.v8i0.1296.
[30] Richards, S.-J., Isufi, K., Wilkins, L. E., Lipecki, J., Fullam, E., Gibson, M. I., … & Fairen-Jimenez, D. (2018). Multivalent antimicrobial polymer nanoparticles target mycobacteria and gram-negative bacteria by distinct mechanisms. Biomacromolecules, 19(1), [256-264]. doi: 10.1021/acs.biomac.7b01561.
[31] Liu, J., Gefen, O., Ronin, I., Bar-Meir, M., & Balaban, N. Q. (2020). Effect of tolerance on the evolution of antibiotic resistance under drug combinations. Science, 367(6474), [200-204]. doi: 10.1126/science.aay3041
[32] Toti, U. S., Guru, B. R., Hali, M., McPharlin, C. M. Susan. M., Wykes, S. M., Panyam, J., & Lehrer, R. I. (2011). Targeted delivery of antibiotics to intracellular chlamydial infections using PLGA nanoparticles. Biomaterials, 32(27), [6606-6613]. doi 10.1016/j.biomaterials.2011.05.038
[33] Sigma-Aldrich. (n.d.). Mesoporous silica. Retrieved from https://www.sigmaaldrich.com/OM/en/technical-documents/technical-article/environmental-testing-and-industrial-hygiene/waste-water-and-process-water-testing/mesoporous-silica
[34] Croissant, J. G., Fatieiev, Y., Almalik, A., & Khashab, N. M. (2018). Mesoporous silica and organosilica nanoparticles: Physical chemistry, biosafety, delivery strategies, and biomedical applications. Advanced Healthcare Materials, 7(4), 1700831. doi: 10.1002/adhm.201700831
[35] Selvarajan, V., Obuobi, S., & Ee, P. L. R. (2020). Silica nanoparticles-a versatile tool for the treatment of bacterial infections. Frontiers in Chemistry, 8, 602. doi: 10.3389/fchem.2020.00602
[36] Doadrio, J. C., Sousa, E. M. B., Izquierdo-Barba, A. L., Perez-Pariente, J., & Vallet-Regí, M. (2006). Functionalization of mesoporous materials with long alkyl chains as a strategy for controlling drug delivery pattern. Journal of Materials Chemistry, 16(5), [462-466]. doi: 10.1039/b510101h
[37] Dinos, G. P., & George, P. (2017). The macrolide antibiotic renaissance. British Journal of Pharmacology, 174(18), [2967-2983]. doi: 10.1111/bph.13936
[38] Aguilera-Correa, M., Gisbert-Garzarán, A., Mediero, M. J., Fernández-Aceñero, D., de-Pablo-Velasco, D., Lozano, D., Esteban, J., & Vallet-Regí, M. (2022). Antibiotic delivery from bone-targeted mesoporous silica nanoparticles for the treatment of osteomyelitis caused by methicillin-resistant Staphylococcus aureus. Acta Biomaterialia, 154, [608-625]. doi: 10.1016/j.actbio.2021.11.017
[39] Kohanski, M. A., Dwyer, D. J., & Collins, J. J. (2010). How antibiotics kill bacteria: From targets to networks. Nature Reviews Microbiology, 8(6), [423-435]. https://doi.org/10.1038/nrmicro2333
[40] Bugg, T. D., & Walsh, C. T. (1992). Intracellular steps of bacterial cell wall peptidoglycan biosynthesis: Enzymology, antibiotics, and antibiotic resistance. Natural Product Reports, 9, [199-215]. https://doi.org/10.1039/NP9920900199
[41] Davis, B. D., Chen, L. L., & Tai, P. C. (1986). Misread protein creates membrane channels: An essential step in the bactericidal action of aminoglycosides. Proceedings of the National Academy of Sciences of the United States of America, 83, [6164-6168]. https://doi.org/10.1073/pnas.83.16.6164
[42] Abo-Shama, U. H., El-Gendy, H., Mousa, W. S., Hamouda, R. A., Yousuf, W. E., Hetta, H. F., & Abdeen, E. E. (2020). Synergistic and Antagonistic Effects of Metal Nanoparticles in Combination with Antibiotics Against Some Reference Strains of Pathogenic Microorganisms. Infection and Drug Resistance, 13, [351-362]. doi: 10.2147/IDR.S234425
[43] Xiu, Z. M., Zhang, Q. B., Puppala, H. L., Colvin, V. L., & Alvarez, P. J. J. (2012). Negligible particle-specific antibacterial activity of silver nanoparticles. Nano Letters, 12(8), [4271-4275]. https://doi.org/10.1021/nl301934w
[44] Sondi, I., & Salopek-Sondi, B. (2004). Silver nanoparticles as antimicrobial agent: A case study on E. coli as a model for gram-negative bacteria. Journal of Colloid and Interface Science, 275(1), [177-182]. https://doi.org/10.1016/j.jcis.2004.02.012
[45] Franci, G., Falanga, A., Galdiero, S., Palomba, L., Rai, M., Morelli, G., & Galdiero, M. (2015). Silver Nanoparticles as Potential Antibacterial Agents. Molecules, 20(5), [8856–8874]. https://doi.org/10.3390/molecules20058856
[46] Guzmán Rodríguez A, Sablón Carrazana M, Rodríguez Tanty C, Malessy MJA, Fuentes G, Cruz LJ. Smart Polymeric Micelles for Anticancer Hydrophobic Drugs. Cancers (Basel). 2022 Dec 20;15(1):4. doi: 10.3390/cancers15010004.
[47] Moss, D. M., Curley, P., Kinvig, H., Hoskins, C., & Owen, A. (2018). The biological challenges and pharmacological opportunities of orally administered nanomedicine delivery. Expert Review of Gastroenterology & Hepatology, 12(3), [223–236]. https://doi.org/10.1080/17474124.2018.1399794
[48] Olivera ME, Manzo RH, Junginger HE, et al. Biowaiver monographs for immediate release solid oral dosage forms: ciprofloxacin hydrochloride. J Pharm Sci. 2011;100(1):[22–33]. doi: 10.1002/jps.22259
[49] Patra, J. K., Das, G., Fraceto, L. F., Campos, E. V. R., Del Pilar Rodriguez-Torres, M., Acosta-Torres, L. S., Diaz-Torres, L. A., Grillo, R., Swamy, M. K., Sharma, S., Habtemariam, S., & Shin, H. (2018). Nano based drug delivery systems: recent developments and future prospects. Journal of Nanobiotechnology, 16(1). https://doi.org/10.1186/s12951-018-0392-8
[50] Gounani, Z., Asadollahi, M. A., Pedersen, J. N., Lyngsø, J., Skov Pedersen, J., Arpanaei, A., & Meyer, R. L. (2019). Mesoporous silica nanoparticles carrying multiple antibiotics provide enhanced synergistic effect and improved biocompatibility. Colloids and Surfaces B: Biointerfaces, 175, [498–508]. https://doi.org/10.1016/j.colsurfb.2018.12.035
[51] Vallet-Regí, M., Schüth, F., Lozano, D., Colilla, M., & Manzano, M. (2022). Engineering mesoporous silica nanoparticles for drug delivery: where are we after two decades? Chemical Society Reviews, 51(13), [5365-5451]. https://doi.org/10.1039/d1cs00659b
[52] Johnston, H. J., Hutchison, G. R., Christensen, F. M., Peters, S., Hankin, S. M., & Stone, V. (2010). A review of the in vivo and in vitro toxicity of silver and gold particulates: Particle attributes and biological mechanisms responsible for the observed toxicity. Critical Reviews in Toxicology, 40(4), [328–346]. https://doi.org/10.3109/10408440903453074
[53] Oberdörster, G., Oberdörster, E., & Oberdörster, J. (2005). Nanotoxicology: An Emerging Discipline Evolving from Studies of Ultrafine Particles. Environmental Health Perspectives, 113(7), [823–839]. https://doi.org/10.1289/ehp.7339
[54] Li, X., Plésiat, P., & Nikaido, H. (2015). The Challenge of Efflux-Mediated Antibiotic Resistance in Gram-Negative Bacteria. Clinical Microbiology Reviews, 28(2), [337–418]. https://doi.org/10.1128/cmr.00117-14
[55] Ajdary, M., Moosavi, M. A., Rahmati, M., Falahati, M., Mahboubi, M., Mandegary, A., Jangjoo, S., Mohammadinejad, R., & Varma, R. S. (2018). Health Concerns of Various Nanoparticles: A Review of Their in Vitro and in Vivo Toxicity. Nanomaterials (Basel), 8(9), 634. https://doi.org/10.3390/nano8090634
[56] Edson, J. A., Kwon, Y.J. (2016). Design, challenge, and promise of stimuli-responsive nanoantibiotics. Nano Converg, 3(1):26. doi: 10.1186/s40580-016-0085-7.
[57] Albers, C. E., Hofstetter, W., Siebenrock, K. A., Landmann, R., Klenke, F.M.(2013) In vitro cytotoxicity of silver NPs on osteoblasts and osteoclasts at antibacterial concentrations. Nanotoxicology. 7(1):30-6. doi: 10.3109/17435390.2011.626538.
[58] Chen, L. Q., Fang, L., Ling, J., Ding, C. Z., Kang, B., & Huang, C. Z. (2015). Nanotoxicity of silver nanoparticles to red blood cells: size dependent adsorption, uptake, and hemolytic activity. Chem Res Toxicol, 28(3), [501–509]. https://doi.org/10.1021/tx500411z
[59] Vimbela GV, Ngo SM, Fraze C, Yang L, Stout DA. Antibacterial properties and toxicity from metallic nanomaterials. Int J Nanomedicine. 2017 May 24;12:3941-3965. doi: 10.2147/IJN.S134526. Erratum in: Int J Nanomedicine. 2018 Oct 16;13:6497.
[60] Sharma, S., Parveen, R., & Chatterji, B. P. (2021). Toxicology of Nanoparticles in Drug Delivery. Current Pathobiology Reports, 9(4), [133-144]. https://doi.org/10.1007/s40139-021-00227-z
[61] Gualtierotti, R., Guarnaccia, L., Beretta, M., Navone, S. E., Campanella, R., Riboni, L., Rampini, P., & Marfia, G. (2017). Modulation of Neuroinflammation in the Central Nervous System: Role of Chemokines and Sphingolipids. Advances in Therapy, 34(2), [396–420]. https://doi.org/10.1007/s12325-016-0474-7
[62] Wnorowska, U., Fiedoruk, K., Piktel, E., et al. (2020). Nanoantibiotics containing membrane-active human cathelicidin LL-37 or synthetic ceragenins attached to the surface of magnetic nanoparticles as novel and innovative therapeutic tools: current status and potential future applications. Journal of Nanobiotechnology, 18, 3. https://doi.org/10.1186/s12951-019-0566-z
[63] Goddard, G., Martin, C. J., Naivar, M. A., Goodwin, P. M., et al.(2006) Single particle high resolution spectral analysis flow cytometry Cytometry Part A 69(8):842-51 DOI:10.1002/cyto.a.20320
[64] Tiambeng, T. N., Roberts, D. S., Zhu, Y., Chen, B., Wu, Z., Mitchell, S. D., … & Kelleher, N. L. (2020). Nanoproteomics enables proteoform-resolved analysis of low-abundance proteins in human serum. Nature Communications, 11(1), 3903. https://doi.org/10.1038/s41467-020-17643-1
[65] Tao, C. (2018). Antimicrobial Activity and Toxicity of Gold Nanoparticles: Research Progress, Challenges and Prospects. Lett. Appl. Microbiol. 67 (6), [537–543]. doi:10.1111/lam.13082
[66] De Jong, W. H., & Borm, P. J. (2008). Drug delivery and nanoparticles: applications and hazards. International Journal of Nanomedicine, 3(2), [133-49]. https://doi.org/10.2147/ijn.s596
[67] Kessler, R. (2011). Engineered nanoparticles in consumer products: understanding a new ingredient. Environmental Health Perspectives, 119, A120–A125. https://doi.org/10.1289/ehp.1103687
[68] Elliott, K.C. (2011). Nanomaterials and the precautionary principle. Environmental Health Perspectives, 119(6), A240. https://doi.org/10.1289/ehp.1103687
[69] Amaro, F., Morón, Á., Díaz, S., Martín-González, A., & Gutiérrez, J.C. (2021). Metallic Nanoparticles—Friends or Foes in the Battle against Antibiotic-Resistant Bacteria? Microorganisms, 9(2), 364. https://doi.org/10.3390/microorganisms9020364
[70] Sydney Rose Addorisio, Shteynberg, R., Dasilva, M., Mixon, J., Mucciarone, K., Vu, L., Arsenault, K., Briand, V., Parker, S., Smith, S., Vise, C., Pina, C. and Laranjo, L. (2022) “Oxidative Stress Response in Bacteria: A Review”, Fine Focus, 8(1), pp. 36–46. doi: 10.33043/FF.8.1
[71] Addorisio, S.R., Shteynberg, R., Dasilva, M., Mixon, J., Mucciarone, K., Vu, L., Arsenault, K., Briand, V., Parker, S., Smith, S., Vise, C., Pina, C., & Laranjo, L. (2022). Oxidative Stress Response in Bacteria: A Review. Fine Focus, 8(1), [36-46]. https://doi.org/10.33043/FF.8.1
[72] Ouyang, K.; Mortimer, M.; Holden, P.A.; Cai, P.; Wu, Y.; Gao, C.; Huang, Q. Towards a better understanding of Pseudomonas putida biofilm formation in the presence of ZnO nanoparticles (NPs): Role of NP concentration. Environ. Int. 2020, 137, 105485. https://doi.org/10.1016/j.envint.2020.105485
[73] Niño-Martínez, N., Salas Orozco, M.F., Martínez-Castañón, G.A., Torres Méndez, F., & Ruiz, F. (2019). Molecular Mechanisms of Bacterial Resistance to Metal and Metal Oxide Nanoparticles. International Journal of Molecular Sciences, 20(11), 2808. https://doi.org/10.3390/ijms20112808