Role of Nanoparticles in Combating Infections
Kanwal Rehman, Muhammad Sajid Hamid Akash
Infections still remain a serious threat to human beings globally. Bacterial infections are one of the major causes of deaths worldwide and increase the overall medical costs, mortality and morbidity due to the development of antimicrobial resistance by means of different mechanisms. Complications related to infectious diseases are being increased day by day, more particularly in developing countries due to limited resources and less availability of the choice of antimicrobial agents. The excessive use of antimicrobial agents creates drug resistance into the pathogens, which demand additional efforts to develop advanced and more effective therapeutic strategies to prevent and treat such kind of infections. So, there was an urgent need to develop new strategies and therapies to cure microbial infections. In response to this need, pharmaceutical scientists are trying their best to design such materials that enhance the biological activity and pharmacokinetic properties of antimicrobial agents against microbial infections. Currently, the best available strategy that can be implemented to prevent the development of drug resistance in pathogens is nanoparticle-based delivery of antimicrobial agents in order to enhance the effectiveness of antimicrobial agents against infections. Nanoparticles have experimentally been proven to have a wide range of antimicrobial potential against various pathogens and an ideal carrier system for intracellular delivery of antimicrobial agents. In this chapter, we have comprehensively summarized the role of polymeric-based nanoparticles for combating the infectious diseases.
Keywords
Antimicrobial Agents, Infections, Polymers, Nanoparticles, Delivery System
Published online 3/25/2019, 30 pages
Citation: Kanwal Rehman, Muhammad Sajid Hamid Akash, Role of Nanoparticles in Combating Infections, Materials Research Foundations, Vol. 47, pp 211-240, 2019
DOI: https://doi.org/10.21741/9781644900130-6
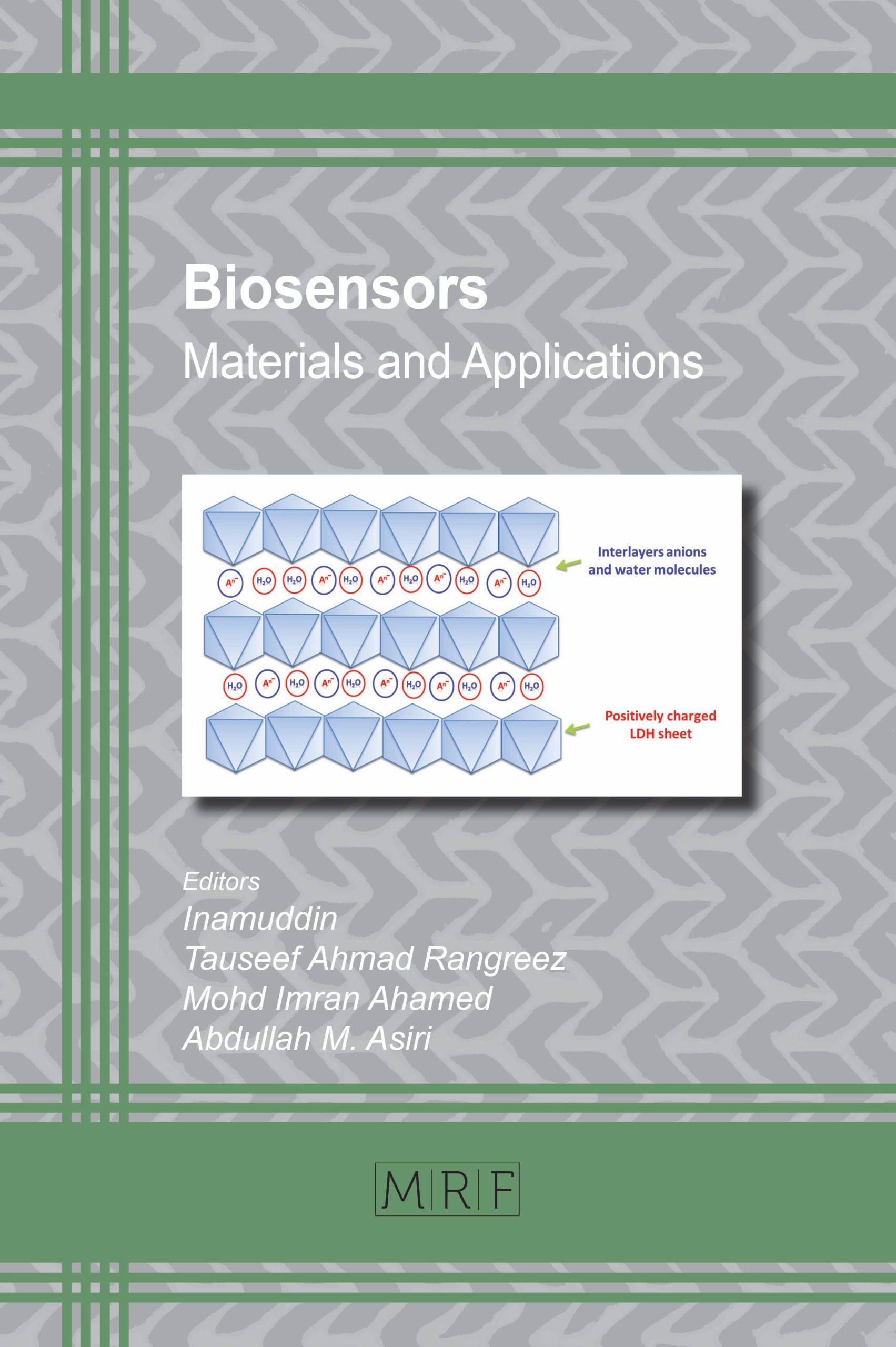
Part of the book on Biosensors
References
[1] M.L. Cohen, Changing patterns of infectious disease, Nature. 406 (2000) 762–767. https://doi.org/10.1038/35021206
[2] G. Taubes, The bacteria fight back, Science (80-. ). 321 (2008) 356–361. https://doi.org/10.1126/science.321.5887.356
[3] A.J. Huh, Y.J. Kwon, “Nanoantibiotics”: A new paradigm for treating infectious diseases using nanomaterials in the antibiotics resistant era, J. Control. Release. 156 (2011) 128–145. https://doi.org/10.1016/j.jconrel.2011.07.002
[4] S.B. Levy, B. Marshall, Antibacterial resistance worldwide: causes, challenges and responses, Nat. Med. 10 (2004) S122–S129. https://doi.org/10.1038/nm1145
[5] G.L. French, The continuing crisis in antibiotic resistance, Int. J. Antimicrob. Agents. 36 (2010) S3–S7. https://doi.org/10.1016/S0924-8579(10)70003-0
[6] A.L. Demain, Antibiotics: Natural products essential to human health, Med. Res. Rev. 29 (2009) 821–842. https://doi.org/10.1002/med.20154
[7] A.S. Pina, A. Hussain, A.C.A. Roque, An historical overview of drug discovery, in: Methods Mol. Biol., 2010: pp. 3–12. https://doi.org/10.1007/978-1-60761-244-5_1
[8] V. Aloush, S. Navon-Venezia, Y. Seigman-Igra, S. Cabili, Y. Carmeli, Multidrug-resistant Pseudomonas aeruginosa: risk factors and clinical impact, Antimicrob. Agents Chemother. 50 (2006) 43–48. https://doi.org/10.1128/AAC.50.1.43-48.2006
[9] V. Manchanda, S. Sanchaita, N. Singh, Multidrug resistant acinetobacter., J. Glob. Infect. Dis. 2 (2010) 291–304. https://doi.org/10.4103/0974-777X.68538
[10] F. Guilhelmelli, N. Vilela, P. Albuquerque, L. da S. Derengowski, I. Silva-Pereira, C.M. Kyaw, Antibiotic development challenges: the various mechanisms of action of antimicrobial peptides and of bacterial resistance, Front. Microbiol. 4 (2013) 353. https://doi.org/10.3389/fmicb.2013.00353
[11] U. Rajchakit, V. Sarojini, Recent developments in antimicrobial-peptide-conjugated gold nanoparticles, Bioconjug. Chem. 28 (2017) 2673–2686. https://doi.org/10.1021/acs.bioconjchem.7b00368
[12] N. Høiby, T. Bjarnsholt, M. Givskov, S. Molin, O. Ciofu, Antibiotic resistance of bacterial biofilms, Int. J. Antimicrob. Agents. 35 (2010) 322–332. https://doi.org/10.1016/j.ijantimicag.2009.12.011
[13] J.A. Otter, K. Vickery, J.T. Walker, E. deLancey Pulcini, P. Stoodley, S.D. Goldenberg, J.A.G. Salkeld, J. Chewins, S. Yezli, J.D. Edgeworth, Surface-attached cells, biofilms and biocide susceptibility: implications for hospital cleaning and disinfection, J. Hosp. Infect. 89 (2015) 16–27. https://doi.org/10.1016/j.jhin.2014.09.008
[14] M.J. Hajipour, K.M. Fromm, A. Akbar Ashkarran, D. Jimenez de Aberasturi, I.R. de Larramendi, T. Rojo, V. Serpooshan, W.J. Parak, M. Mahmoudi, Antibacterial properties of nanoparticles, Trends Biotechnol. 30 (2012) 499–511. https://doi.org/10.1016/j.tibtech.2012.06.004
[15] P.A. Patel, V.B. Patravale, AmbiOnp: solid lipid nanoparticles of amphotericin B for oral administration., J. Biomed. Nanotechnol. 7 (2011) 632–9. https://www.ncbi.nlm.nih.gov/pubmed/22195480 (accessed January 2, 2019)
[16] M.B. Chaudhari, P.P. Desai, P.A. Patel, V.B. Patravale, Solid lipid nanoparticles of amphotericin B (AmbiOnp): in vitro and in vivo assessment towards safe and effective oral treatment module, Drug Deliv. Transl. Res. 6 (2015) 354–64. https://doi.org/10.1007/s13346-015-0267-6
[17] D.M. Casa, T.C.M.M. Carraro, L.E.A. de Camargo, L.F. Dalmolin, N.M. Khalil, R.M. Mainardes, Poly(L-lactide) nanoparticles reduce amphotericin b cytotoxicity and maintain its in vitro antifungal activity., J. Nanosci. Nanotechnol. 15 (2015) 848–54. https://www.ncbi.nlm.nih.gov/pubmed/26328449 (accessed January 2, 2019)
[18] R. Singh, M.S. Smitha, S.P. Singh, The role of nanotechnology in combating multi-drug resistant bacteria., J. Nanosci. Nanotechnol. 14 (2014) 4745–56. https://www.ncbi.nlm.nih.gov/pubmed/24757944 (accessed January 2, 2019)
[19] C. Noguera, Physics and chemistry at oxide surfaces, Cambridge University Press, 1996
[20] H.H. Kung, Transition metal oxides : surface chemistry and catalysis, Elsevier, 1989.
[21] J.M. Vohs, The surface science of metal oxides. By V. E. Henrich and P. A. Cox, Cambridge University Press, Cambridge, U.K., 1994, 464 pp. hardcover $99.95; paperback $39.95, AIChE J. 44 (1998) 502–503. https://doi.org/10.1002/aic.690440230
[22] J.A. Rodríguez, M. Fernández Garcia, Synthesis, properties, and applications of oxide nanomaterials, Wiley-Interscience, 2007
[23] M. Fernández-García, A. Martínez-Arias, J.C. Hanson, J.A. Rodriguez, Nanostructured oxides in chemistry: characterization and properties, (2004). https://doi.org/10.1021/CR030032F
[24] S.D. Puckett, E. Taylor, T. Raimondo, T.J. Webster, The relationship between the nanostructure of titanium surfaces and bacterial attachment, Biomaterials. 31 (2010) 706–713. https://doi.org/10.1016/j.biomaterials.2009.09.081
[25] K.M. Tarquinio, N.K. Kothurkar, D.Y. Goswami, R.C. Sanders, A.L. Zaritsky, A.M. LeVine, Bactericidal effects of silver plus titanium dioxide-coated endotracheal tubes on Pseudomonas aeruginosa and Staphylococcus aureus., Int. J. Nanomedicine. 5 (2010) 177–83. https://www.ncbi.nlm.nih.gov/pubmed/20463933 (accessed January 2, 2019)
[26] N. Tran, A. Mir, D. Mallik, A. Sinha, S. Nayar, T.J. Webster, Bactericidal effect of iron oxide nanoparticles on Staphylococcus aureus., Int. J. Nanomedicine. 5 (2010) 277–83. https://www.ncbi.nlm.nih.gov/pubmed/20463943 (accessed January 2, 2019)
[27] P.A. Tran, T.J. Webster, Selenium nanoparticles inhibit Staphylococcus aureus growth., Int. J. Nanomedicine. 6 (2011) 1553–8. https://doi.org/10.2147/IJN.S21729
[28] S.M. Moghimi, A.C. Hunter, T.L. Andresen, Factors controlling nanoparticle pharmacokinetics: an integrated analysis and perspective, Annu. Rev. Pharmacol. Toxicol. 52 (2012) 481–503. https://doi.org/10.1146/annurev-pharmtox-010611-134623
[29] A.E. Nel, L. Mädler, D. Velegol, T. Xia, E.M. V. Hoek, P. Somasundaran, F. Klaessig, V. Castranova, M. Thompson, Understanding biophysicochemical interactions at the nano–bio interface, Nat. Mater. 8 (2009) 543–557. https://doi.org/10.1038/nmat2442
[30] N. Khlebtsov, L. Dykman, Biodistribution and toxicity of engineered gold nanoparticles: a review of in vitro and in vivo studies., Chem. Soc. Rev. 40 (2011) 1647–71. https://doi.org/10.1039/c0cs00018c
[31] M.-C. Bowman, T.E. Ballard, C.J. Ackerson, D.L. Feldheim, D.M. Margolis, C. Melander, Inhibition of HIV Fusion with Multivalent Gold Nanoparticles, J. Am. Chem. Soc. 130 (2008) 6896–6897. https://doi.org/10.1021/ja710321g
[32] O.M. Koo, I. Rubinstein, H. Onyuksel, Role of nanotechnology in targeted drug delivery and imaging: a concise review, Nanomedicine Nanotechnology, Biol. Med. 1 (2005) 193–212. https://doi.org/10.1016/j.nano.2005.06.004
[33] R.T. Sadikot, I. Rubinstein, Long-acting, multi-targeted nanomedicine: addressing unmet medical need in acute lung injury, J. Biomed. Nanotechnol. 5 (2009) 614–619. https://doi.org/10.1166/jbn.2009.1078
[34] R.T. Sadikot, Peptide Nanomedicines for treatment of acute lung injury, in: Methods Enzymol., 2012: pp. 315–324. https://doi.org/10.1016/B978-0-12-391860-4.00016-1
[35] K.S. Brandenburg, I. Rubinstein, R.T. Sadikot, H. Önyüksel, Polymyxin B self-associated with phospholipid nanomicelles, Pharm. Dev. Technol. 17 (2012) 654–660. https://doi.org/10.3109/10837450.2011.572893
[36] P. Couvreur, C. Vauthier, Nanotechnology: intelligent design to treat complex disease, Pharm. Res. 23 (2006) 1417–1450. https://doi.org/10.1007/s11095-006-0284-8
[37] P.R. Lockman, R.J. Mumper, M.A. Khan, D.D. Allen, Nanoparticle technology for drug delivery across the blood-brain barrier, Drug Dev. Ind. Pharm. 28 (2002) 1–13. https://doi.org/10.1081/DDC-120001481
[38] T.K.M. Mbela ’, J.H. Poupaert ’, P. Dumont, Poly( diethylmethylidene malonate) nanoparticles as primaquine delivery system to liver, 1992
[39] M.S.H. Akash, K. Rehman, Recent progress in biomedical applications of Pluronic (PF127): Pharmaceutical perspectives, J. Control. Release. 209 (2015) 120–138. https://doi.org/10.1016/j.jconrel.2015.04.032
[40] M.S.H. Akash, K. Rehman, S. Chen, Pluronic F127-based thermosensitive gels for delivery of therapeutic proteins and peptides, Polym. Rev. 54 (2014) 573–597. https://doi.org/10.1080/15583724.2014.927885
[41] M.S.H. Akash, K. Rehman, S. Chen, Natural and synthetic polymers as drug carriers for delivery of therapeutic proteins, Polym. Rev. 55 (2015) 371–406. https://doi.org/10.1080/15583724.2014.995806
[42] M.S.H. Akash, K. Rehman, S. Chen, Polymeric-based particulate systems for delivery of therapeutic proteins, Pharm. Dev. Technol. 21 (2016) 367–378. https://doi.org/10.3109/10837450.2014.999785
[43] M.S.H. Akash, K. Rehman, M. Tariq, S. Chen, Development of therapeutic proteins: Advances and challenges. Turk J Biol. 2015;39(3):343-58
[44] R.A. Petros, J.M. DeSimone, Strategies in the design of nanoparticles for therapeutic applications, Nat. Rev. Drug Discov. 9 (2010) 615–627. https://doi.org/10.1038/nrd2591
[45] M.E. Davis, Z. Chen, D.M. Shin, Nanoparticle therapeutics: an emerging treatment modality for cancer, Nat. Rev. Drug Discov. 7 (2008) 771–782. https://doi.org/10.1038/nrd2614
[46] L. Zhang, D. Pornpattananangku, C.-M.J. Hu, C.-M. Huang, Development of nanoparticles for antimicrobial drug delivery., Curr. Med. Chem. 17 (2010) 585–94
[47] M.S.H. Akash, K. Rehman, S. Chen, IL-1Ra and its delivery strategies: inserting the association in perspective, Pharm. Res. 30 (2013) 2951–2966. https://doi.org/10.1007/s11095-013-1118-0
[48] M.S.H. Akash, K. Rehman, N. Li, J.-Q. Gao, H. Sun, S. Chen, Sustained delivery of IL-1Ra from Pluronic F127-based thermosensitive gel prolongs its therapeutic potentials, Pharm. Res. 29 (2012) 3475–3485. https://doi.org/10.1007/s11095-012-0843-0
[49] H.M. Mansour, Y.-S. Rhee, X. Wu, Nanomedicine in pulmonary delivery., Int. J. Nanomedicine. 4 (2009) 299–319. https://www.ncbi.nlm.nih.gov/pubmed/20054434 (accessed January 2, 2019)
[50] W. Gao, S. Thamphiwatana, P. Angsantikul, L. Zhang, Nanoparticle approaches against bacterial infections, Wiley Interdiscip. Rev. Nanomedicine Nanobiotechnology. 6 (2014) 532–547. https://doi.org/10.1002/wnan.1282
[51] R.Y. Pelgrift, A.J. Friedman, Nanotechnology as a therapeutic tool to combat microbial resistance, Adv. Drug Deliv. Rev. 65 (2013) 1803–1815. https://doi.org/10.1016/j.addr.2013.07.011
[52] S.M. Dizaj, F. Lotfipour, M. Barzegar-Jalali, M.H. Zarrintan, K. Adibkia, Antimicrobial activity of the metals and metal oxide nanoparticles, Mater. Sci. Eng. C. 44 (2014) 278–284. https://doi.org/10.1016/j.msec.2014.08.031
[53] B. Fadeel, Nanosafety: towards safer design of nanomedicines, J. Intern. Med. 274 (2013) 578–580. https://doi.org/10.1111/joim.12137
[54] M. Banerjee, S. Mallick, A. Paul, A. Chattopadhyay, S.S. Ghosh, Heightened reactive oxygen species generation in the antimicrobial activity of a three component iodinated chitosan−silver nanoparticle composite, Langmuir. 26 (2010) 5901–5908. https://doi.org/10.1021/la9038528
[55] F. Martinez-Gutierrez, P.L. Olive, A. Banuelos, E. Orrantia, N. Nino, E.M. Sanchez, F. Ruiz, H. Bach, Y. Av-Gay, Synthesis, characterization, and evaluation of antimicrobial and cytotoxic effect of silver and titanium nanoparticles, Nanomedicine Nanotechnology, Biol. Med. 6 (2010) 681–688. https://doi.org/10.1016/j.nano.2010.02.001
[56] S. Ghosh, R. Kaushik, K. Nagalakshmi, S.L. Hoti, G.A. Menezes, B.N. Harish, H.N. Vasan, Antimicrobial activity of highly stable silver nanoparticles embedded in agar-agar matrix as a thin film., Carbohydr. Res. 345 (2010) 2220–7. https://doi.org/10.1016/j.carres.2010.08.001
[57] S. Shrivastava, T. Bera, A. Roy, G. Singh, P. Ramachandrarao, D. Dash, Characterization of enhanced antibacterial effects of novel silver nanoparticles, Nanotechnology. 18 (2007) 225103. https://doi.org/10.1088/0957-4484/18/22/225103
[58] A.R. Shahverdi, A. Fakhimi, H.R. Shahverdi, S. Minaian, Synthesis and effect of silver nanoparticles on the antibacterial activity of different antibiotics against Staphylococcus aureus and Escherichia coli, Nanomedicine Nanotechnology, Biol. Med. 3 (2007) 168–171. https://doi.org/10.1016/j.nano.2007.02.001
[59] J.S. Kim, E. Kuk, K.N. Yu, J.-H. Kim, S.J. Park, H.J. Lee, S.H. Kim, Y.K. Park, Y.H. Park, C.-Y. Hwang, Y.-K. Kim, Y.-S. Lee, D.H. Jeong, M.-H. Cho, Antimicrobial effects of silver nanoparticles, Nanomedicine Nanotechnology, Biol. Med. 3 (2007) 95–101. https://doi.org/10.1016/j.nano.2006.12.001
[60] Y. Ma, T. Zhou, C. Zhao, Preparation of chitosan-nylon-6 blended membranes containing silver ions as antibacterial materials., Carbohydr. Res. 343 (2008) 230–7. https://doi.org/10.1016/j.carres.2007.11.006
[61] P. Sanpui, A. Murugadoss, P. Prasad, S. Ghosh, A. Chattopadhyay, The antibacterial properties of a novel chitosan–Ag-nanoparticle composite, Int. J. Food Microbiol. 124 (2008) 142–146. https://doi.org/10.1016/j.ijfoodmicro.2008.03.004
[62] L. Qi, Z. Xu, X. Jiang, C. Hu, X. Zou, Preparation and antibacterial activity of chitosan nanoparticles, (2004). https://doi.org/10.1016/j.carres.2004.09.007
[63] S. Chadwick, C. Kriegel, M. Amiji, Nanotechnology solutions for mucosal immunization, Adv. Drug Deliv. Rev. 62 (2010) 394–407. https://doi.org/10.1016/j.addr.2009.11.012
[64] A.J. Friedman, G. Han, M.S. Navati, M. Chacko, L. Gunther, A. Alfieri, J.M. Friedman, Sustained release nitric oxide releasing nanoparticles: Characterization of a novel delivery platform based on nitrite containing hydrogel/glass composites, Nitric Oxide. 19 (2008) 12–20. https://doi.org/10.1016/j.niox.2008.04.003
[65] M. Potara, E. Jakab, A. Damert, O. Popescu, V. Canpean, S. Astilean, Synergistic antibacterial activity of chitosan–silver nanocomposites on Staphylococcus aureus, Nanotechnology. 22 (2011) 135101. https://doi.org/10.1088/0957-4484/22/13/135101
[66] M. Rai, A. Yadav, A. Gade, Silver nanoparticles as a new generation of antimicrobials, Biotechnol. Adv. 27 (2009) 76–83. https://doi.org/10.1016/J.BIOTECHADV.2008.09.002
[67] S. Pal, Y.K. Tak, J.M. Song, Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A study of the Gram-negative bacterium Escherichia coli., Appl. Environ. Microbiol. 73 (2007) 1712–20. https://doi.org/10.1128/AEM.02218-06
[68] Q.L. Feng, J. Wu, G.Q. Chen, F.Z. Cui, T.N. Kim, J.O. Kim, A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus., J. Biomed. Mater. Res. 52 (2000) 662–8
[69] G. Applerot, A. Lipovsky, R. Dror, N. Perkas, Y. Nitzan, R. Lubart, A. Gedanken, Enhanced antibacterial activity of nanocrystalline ZnO due to increased ROS-mediated cell injury, Adv. Funct. Mater. 19 (2009) 842–852. https://doi.org/10.1002/adfm.200801081
[70] N. Jones, B. Ray, K.T. Ranjit, A.C. Manna, Antibacterial activity of ZnO nanoparticle suspensions on a broad spectrum of microorganisms, FEMS Microbiol. Lett. 279 (2008) 71–76. https://doi.org/10.1111/j.1574-6968.2007.01012.x
[71] E. Taylor, T.J. Webster, Reducing infections through nanotechnology and nanoparticles., Int. J. Nanomedicine. 6 (2011) 1463–73. https://doi.org/10.2147/IJN.S22021
[72] A. Nanda, M. Saravanan, Biosynthesis of silver nanoparticles from Staphylococcus aureus and its antimicrobial activity against MRSA and MRSE, Nanomedicine Nanotechnology, Biol. Med. 5 (2009) 452–456. https://doi.org/10.1016/j.nano.2009.01.012
[73] D.S. Balaji, S. Basavaraja, R. Deshpande, D.B. Mahesh, B.K. Prabhakar, A. Venkataraman, Extracellular biosynthesis of functionalized silver nanoparticles by strains of Cladosporium cladosporioides fungus, Colloids Surfaces B Biointerfaces. 68 (2009) 88–92. https://doi.org/10.1016/j.colsurfb.2008.09.022
[74] S. Basavaraja, S.D. Balaji, A. Lagashetty, A.H. Rajasab, A. Venkataraman, Extracellular biosynthesis of silver nanoparticles using the fungus Fusarium semitectum, Mater. Res. Bull. 43 (2008) 1164–1170. https://doi.org/10.1016/J.MATERRESBULL.2007.06.020
[75] J.D. Holmes, P.R. Smith, R. Evans-Gowing, D.J. Richardson, D.A. Russell, J.R. Sodeau, Energy-dispersive X-ray analysis of the extracellular cadmium sulfide crystallites of Klebsiella aerogenes, Arch. Microbiol. 163 (1995) 143–147. https://doi.org/10.1007/BF00381789
[76] M. Saravanan, A. Nanda, Extracellular synthesis of silver bionanoparticles from Aspergillus clavatus and its antimicrobial activity against MRSA and MRSE, Colloids Surfaces B Biointerfaces. 77 (2010) 214–218. https://doi.org/10.1016/j.colsurfb.2010.01.026
[77] K. Chaloupka, Y. Malam, A.M. Seifalian, Nanosilver as a new generation of nanoproduct in biomedical applications, Trends Biotechnol. 28 (2010) 580–588. https://doi.org/10.1016/j.tibtech.2010.07.006
[78] N.G. Durmus, E.N. Taylor, K.M. Kummer, T.J. Webster, Enhanced efficacy of superparamagnetic iron oxide nanoparticles against antibiotic-resistant biofilms in the presence of metabolites, Adv. Mater. 25 (2013) 5706–5713. https://doi.org/10.1002/adma.201302627
[79] G.D. Savi, M.M. da Silva Paula, J.C. Possato, T. Barichello, D. Castagnaro, V.M. Scussel, Biological activity of gold nanoparticles towards filamentous pathogenic fungi, J. Nano Res. 20 (2012) 11–20. https://doi.org/10.4028/www.scientific.net/JNanoR.20.11
[80] L. Brunet, D.Y. Lyon, E.M. Hotze, P.J.J. Alvarez, M.R. Wiesner, Comparative Photoactivity and antibacterial properties of C 60 fullerenes and titanium dioxide nanoparticles, Environ. Sci. Technol. 43 (2009) 4355–4360. https://doi.org/10.1021/es803093t
[81] M. Premanathan, K. Karthikeyan, K. Jeyasubramanian, G. Manivannan, Selective toxicity of ZnO nanoparticles toward Gram-positive bacteria and cancer cells by apoptosis through lipid peroxidation, Nanomedicine Nanotechnology, Biol. Med. 7 (2011) 184–192. https://doi.org/10.1016/j.nano.2010.10.001
[82] J. Ma, Z. Xiong, T. David Waite, W.J. Ng, X.S. Zhao, Enhanced inactivation of bacteria with silver-modified mesoporous TiO2 under weak ultraviolet irradiation, Microporous Mesoporous Mater. 144 (2011) 97–104. https://doi.org/10.1016/j.micromeso.2011.03.040
[83] E. Torres-Sangiao, A. Holban, M. Gestal, Advanced nanobiomaterials: vaccines, diagnosis and treatment of infectious diseases, Molecules. 21 (2016) 867. https://doi.org/10.3390/molecules21070867
[84] A. Raghunath, E. Perumal, Metal oxide nanoparticles as antimicrobial agents: a promise for the future, Int. J. Antimicrob. Agents. 49 (2017) 137–152. https://doi.org/10.1016/j.ijantimicag.2016.11.011
[85] B. Sarkar, A. Mahanty, S.P. Netam, S. Mishra, N. Pradhan, M. Samanta, Inhibitory role of silver nanoparticles against important fish pathogen, Aeromonas hydrophila, Int. J. Nanomater. Biostructures. 2 (2012) 70–74. https://www.urpjournals.com (accessed January 3, 2019)
[86] V. Ahmed, J. Kumar, M. Kumar, M.B. Chauhan, M. Vij, M. Ganguli, N.S. Chauhan, Synthesis, characterization of penicillin G capped silver nanoconjugates to combat β-lactamase resistance in infectious microorganism., J. Biotechnol. 163 (2013) 419–24. https://doi.org/10.1016/j.jbiotec.2012.12.002
[87] A. Travan, C. Pelillo, I. Donati, E. Marsich, M. Benincasa, T. Scarpa, S. Semeraro, G. Turco, R. Gennaro, S. Paoletti, Non-cytotoxic silver nanoparticle-polysaccharide nanocomposites with antimicrobial activity, Biomacromolecules. 10 (2009) 1429–1435. https://doi.org/10.1021/bm900039x
[88] K. Madhumathi, P.T. Sudheesh Kumar, S. Abhilash, V. Sreeja, H. Tamura, K. Manzoor, S. V. Nair, R. Jayakumar, Development of novel chitin/nanosilver composite scaffolds for wound dressing applications, J. Mater. Sci. Mater. Med. 21 (2010) 807–813. https://doi.org/10.1007/s10856-009-3877-z
[89] B. Marta, E. Jakab, M. Potara, T. Simon, F. Imre-Lucaci, L. Barbu-Tudoran, O. Popescu, S. Astilean, Pluronic-coated silver nanoprisms: Synthesis, characterization and their antibacterial activity, Colloids Surfaces A Physicochem. Eng. Asp. 441 (2014) 77–83. https://doi.org/10.1016/J.COLSURFA.2013.08.076
[90] R. Dobrucka, J. Długaszewska, Biosynthesis and antibacterial activity of ZnO nanoparticles using Trifolium pratense flower extract, Saudi J. Biol. Sci. 23 (2016) 517–523. https://doi.org/10.1016/j.sjbs.2015.05.016
[91] L.S. Reddy, M.M. Nisha, M. Joice, P.N. Shilpa, Antimicrobial activity of zinc oxide (ZnO) nanoparticle against Klebsiella pneumoniae, Pharm. Biol. 52 (2014) 1388–1397. https://doi.org/10.3109/13880209.2014.893001
[92] Y. Liu, L. He, A. Mustapha, H. Li, Z.Q. Hu, M. Lin, Antibacterial activities of zinc oxide nanoparticles against Escherichia coli O157:H7, J. Appl. Microbiol. 107 (2009) 1193–1201. https://doi.org/10.1111/j.1365-2672.2009.04303.x
[93] Y. Xie, Y. He, P.L. Irwin, T. Jin, X. Shi, Antibacterial activity and mechanism of action of zinc oxide nanoparticles against Campylobacter jejuni., Appl. Environ. Microbiol. 77 (2011) 2325–31. https://doi.org/10.1128/AEM.02149-10
[94] A. Sirelkhatim, S. Mahmud, A. Seeni, N.H.M. Kaus, L.C. Ann, S.K.M. Bakhori, H. Hasan, D. Mohamad, Review on Zinc oxide nanoparticles: antibacterial activity and toxicity mechanism, Nano-Micro Lett. 7 (2015) 219–242. https://doi.org/10.1007/s40820-015-0040-x
[95] A. Giasuddin, K. Jhuma, A.M. Haq, Use of gold nanoparticles in diagnostics, surgery and medicine: a review, Bangladesh J. Med. Biochem. 5 (2013) 56–60. https://doi.org/10.3329/bjmb.v5i2.13346
[96] S. Jain, D.G. Hirst, J.M. O’Sullivan, Gold nanoparticles as novel agents for cancer therapy, Br. J. Radiol. 85 (2012) 101–113. https://doi.org/10.1259/bjr/59448833
[97] A. Mesbahi, A review on gold nanoparticles radiosensitization effect in radiation therapy of cancer., Reports Pract. Oncol. Radiother. J. Gt. Cancer Cent. Pozn. Polish Soc. Radiat. Oncol. 15 (2010) 176–80. https://doi.org/10.1016/j.rpor.2010.09.001
[98] Jacob D. Gibson, and Bishnu P. Khanal, E.R. Zubarev, Paclitaxel-functionalized gold nanoparticles, JACS (2007). https://doi.org/10.1021/JA075181K
[99] M.M. Mohamed, S.A. Fouad, H.A. Elshoky, G.M. Mohammed, T.A. Salaheldin, Antibacterial effect of gold nanoparticles against Corynebacterium pseudotuberculosis, Int. J. Vet. Sci. Med. 5 (2017) 23–29. https://doi.org/10.1016/J.IJVSM.2017.02.003
[100] S. Shamaila, N. Zafar, S. Riaz, R. Sharif, J. Nazir, S. Naseem, Gold nanoparticles: an efficient antimicrobial agent against enteric bacterial human pathogen., Nanomater. (Basel, Switzerland). 6 (2016). https://doi.org/10.3390/nano6040071
[101] J.A. Lemire, J.J. Harrison, R.J. Turner, Antimicrobial activity of metals: mechanisms, molecular targets and applications, Nat. Rev. Microbiol. 11 (2013) 371–384. https://doi.org/10.1038/nrmicro3028
[102] M. Seong, D.G. Lee, Reactive oxygen species-independent apoptotic pathway by gold nanoparticles in Candida albicans., Microbiol. Res. 207 (2018) 33–40. https://doi.org/10.1016/j.micres.2017.11.003
[103] N. Mahmoud, A. Alkilany, E. Khalil, A. Al-Bakri, Antibacterial activity of gold nanorods against Staphylococcus aureus and Propionibacterium acnes: misinterpretations and artifacts, Int. J. Nanomedicine. Volume 12 (2017) 7311–7322. https://doi.org/10.2147/IJN.S145531
[104] J.P. Ruparelia, A.K. Chatterjee, S.P. Duttagupta, S. Mukherji, Strain specificity in antimicrobial activity of silver and copper nanoparticles, Acta Biomater. 4 (2008) 707–716. https://doi.org/10.1016/j.actbio.2007.11.006
[105] G. Ren, D. Hu, E.W.C. Cheng, M.A. Vargas-Reus, P. Reip, R.P. Allaker, Characterisation of copper oxide nanoparticles for antimicrobial applications, Int. J. Antimicrob. Agents. 33 (2009) 587–590. https://doi.org/10.1016/j.ijantimicag.2008.12.004
[106] M. Ahamed, H.A. Alhadlaq, M.A.M. Khan, P. Karuppiah, N.A. Al-Dhabi, Synthesis, characterization, and antimicrobial activity of copper oxide nanoparticles, J. Nanomater. 2014 (2014) 1–4. https://doi.org/10.1155/2014/637858
[107] G. Applerot, J. Lellouche, A. Lipovsky, Y. Nitzan, R. Lubart, A. Gedanken, E. Banin, Understanding the antibacterial mechanism of CuO Nanoparticles: revealing the route of induced oxidative stress, Small. 8 (2012) 3326–3337. https://doi.org/10.1002/smll.201200772
[108] H.R. Ashjari, M.S.S. Dorraji, V. Fakhrzadeh, H. Eslami, M.H. Rasoulifard, M. Rastgouy-Houjaghan, P. Gholizadeh, H.S. Kafil, Starch-based polyurethane/CuO nanocomposite foam: Antibacterial effects for infection control., Int. J. Biol. Macromol. 111 (2018) 1076–1082. https://doi.org/10.1016/j.ijbiomac.2018.01.137
[109] D. Devipriya, S.M. Roopan, Cissus quadrangularis mediated ecofriendly synthesis of copper oxide nanoparticles and its antifungal studies against Aspergillus niger, Aspergillus flavus, Mater. Sci. Eng. C. 80 (2017) 38–44. https://doi.org/10.1016/j.msec.2017.05.130
[110] Q. Maqbool, S. Iftikhar, M. Nazar, F. Abbas, A. Saleem, T. Hussain, R. Kausar, S. Anwaar, N. Jabeen, Green fabricated CuO nanobullets via Olea europaea leaf extract shows auspicious antimicrobial potential, IET Nanobiotechnology. 11 (2017) 463–468. https://doi.org/10.1049/iet-nbt.2016.0125
[111] P.K. Stoimenov, R.L. Klinger, G.L. Marchin, K.J. Klabunde, Metal oxide nanoparticles as bactericidal agents, (2002). https://doi.org/10.1021/LA0202374
[112] J. Lellouche, E. Kahana, S. Elias, A. Gedanken, E. Banin, Antibiofilm activity of nanosized magnesium fluoride, Biomaterials. 30 (2009) 5969–5978. https://doi.org/10.1016/J.BIOMATERIALS.2009.07.037
[113] A. Landriscina, J. Rosen, A.J. Friedman, Biodegradable chitosan nanoparticles in drug delivery for infectious disease., Nanomedicine (Lond). 10 (2015) 1609–19. https://doi.org/10.2217/nnm.15.7
[114] V. Saharan, A. Mehrotra, R. Khatik, P. Rawal, S.S. Sharma, A. Pal, Synthesis of chitosan based nanoparticles and their in vitro evaluation against phytopathogenic fungi, Int. J. Biol. Macromol. 62 (2013) 677–683. https://doi.org/10.1016/j.ijbiomac.2013.10.012
[115] B. Jamil, H. Habib, S. Abbasi, H. Nasir, A. Rahman, A. Rehman, H. Bokhari, M. Imran, Cefazolin loaded chitosan nanoparticles to cure multi drug resistant Gram-negative pathogens., Carbohydr. Polym. 136 (2016) 682–91. https://doi.org/10.1016/j.carbpol.2015.09.078
[116] K. Blecher, A. Nasir, A. Friedman, The growing role of nanotechnology in combating infectious disease, Virulence. 2 (2011) 395–401. https://doi.org/10.4161/viru.2.5.17035
[117] C.T. Tsao, C.H. Chang, Y.Y. Lin, M.F. Wu, J.-L. Wang, J.L. Han, K.H. Hsieh, Antibacterial activity and biocompatibility of a chitosan-gamma-poly(glutamic acid) polyelectrolyte complex hydrogel., Carbohydr. Res. 345 (2010) 1774–80. https://doi.org/10.1016/j.carres.2010.06.002
[118] M.A. Aziz, J.D. Cabral, H.J.L. Brooks, S.C. Moratti, L.R. Hanton, Antimicrobial properties of a chitosan dextran-based hydrogel for surgical use., Antimicrob. Agents Chemother. 56 (2012) 280–7. https://doi.org/10.1128/AAC.05463-11
[119] M. Qasim, D.-J. Lim, H. Park, D. Na, Nanotechnology for diagnosis and treatment of infectious diseases, J. Nanosci. Nanotechnol. 14 (2014) 7374–7387. https://doi.org/10.1166/jnn.2014.9578
[120] L. Zhan, S.J. Zhen, X.Y. Wan, P.F. Gao, C.Z. Huang, A sensitive surface-enhanced Raman scattering enzyme-catalyzed immunoassay of respiratory syncytial virus., Talanta. 148 (2016) 308–12. https://doi.org/10.1016/j.talanta.2015.10.081
[121] L. Chen, N. Mungroo, L. Daikuara, S. Neethirajan, Label-free NIR-SERS discrimination and detection of foodborne bacteria by in situ synthesis of Ag colloids, J. Nanobiotechnology. 13 (2015) 45. https://doi.org/10.1186/s12951-015-0106-4
[122] Z. Wang, N. Duan, J. Li, J. Ye, S. Ma, G. Le, Ultrasensitive chemiluminescent immunoassay of Salmonella with silver enhancement of nanogold labels, Luminescence. 26 (2011) 136–141. https://doi.org/10.1002/bio.1196
[123] J. Huang, Z. Xie, Z. Xie, S. Luo, L. Xie, L. Huang, Q. Fan, Y. Zhang, S. Wang, T. Zeng, Silver nanoparticles coated graphene electrochemical sensor for the ultrasensitive analysis of avian influenza virus H7, Anal. Chim. Acta. 913 (2016) 121–127. https://doi.org/10.1016/j.aca.2016.01.050
[124] J. Li, T. Qin, X.X. Jia, A.H. Deng, X. Zhang, W.H. Fan, S.D. Huo, T.Y. Wen, W.J. Liu, Rapid Identification of Legionella Pathogenicity by Surface-Enhanced Raman Spectroscopy., Biomed. Environ. Sci. 28 (2015) 437–44. https://doi.org/10.3967/bes2015.061
[125] A. Sivanesan, E. Witkowska, W. Adamkiewicz, Ł. Dziewit, A. Kamińska, J. Waluk, Nanostructured silver–gold bimetallic SERS substrates for selective identification of bacteria in human blood, Analyst. 139 (2014) 1037. https://doi.org/10.1039/c3an01924a
[126] B. Veigas, A.R. Fernandes, P. V Baptista, AuNPs for identification of molecular signatures of resistance., Front. Microbiol. 5 (2014) 455. https://doi.org/10.3389/fmicb.2014.00455
[127] H. Deng, X. Zhang, A. Kumar, G. Zou, X. Zhang, X.-J. Liang, Long genomic DNA amplicons adsorption onto unmodified gold nanoparticles for colorimetric detection of Bacillus anthracis, Chem. Commun. 49 (2013) 51–53. https://doi.org/10.1039/C2CC37037A
[128] K. Kalidasan, J.L. Neo, M. Uttamchandani, Direct visual detection of Salmonella genomic DNA using gold nanoparticles, Mol. Biosyst. 9 (2013) 618. https://doi.org/10.1039/c3mb25527a
[129] M.A.F. Khalil, H.M.E. Azzazy, A.S. Attia, A.G.M. Hashem, A sensitive colorimetric assay for identification of Acinetobacter baumannii using unmodified gold nanoparticles, J. Appl. Microbiol. 117 (2014) 465–471. https://doi.org/10.1111/jam.12546
[130] B. Veigas, P. Pedrosa, F.F. Carlos, L. Mancio-Silva, A.R. Grosso, E. Fortunato, M.M. Mota, P. V Baptista, One nanoprobe, two pathogens: gold nanoprobes multiplexing for point-of-care., J. Nanobiotechnology. 13 (2015) 48. https://doi.org/10.1186/s12951-015-0109-1
[131] P. Pedrosa, Gold nanoprobes for multi loci assessment of multi-drug resistant tuberculosis, Tuberculosis. 94 (2014)
[132] X. Li, H. Kong, R. Mout, K. Saha, D.F. Moyano, S.M. Robinson, S. Rana, X. Zhang, M.A. Riley, V.M. Rotello, Rapid identification of bacterial biofilms and biofilm wound models using a multichannel nanosensor, ACS Nano. 8 (2014) 12014–12019. https://doi.org/10.1021/nn505753s
[133] C. Pöhlmann, I. Dieser, M. Sprinzl, A lateral flow assay for identification of Escherichia coli by ribosomal RNA hybridisation, Analyst. 139 (2014) 1063. https://doi.org/10.1039/c3an02059b
[134] J. Zhao, S. Tang, J. Storhoff, S. Marla, Y.P. Bao, X. Wang, E.Y. Wong, V. Ragupathy, Z. Ye, I.K. Hewlett, Multiplexed, rapid detection of H5N1 using a PCR-free nanoparticle-based genomic microarray assay, BMC Biotechnol. 10 (2010) 74. https://doi.org/10.1186/1472-6750-10-74
[135] M. Chen, Z. Yu, D. Liu, T. Peng, K. Liu, S. Wang, Y. Xiong, H. Wei, H. Xu, W. Lai, Dual gold nanoparticle lateflow immunoassay for sensitive detection of Escherichia coli O157:H7, Anal. Chim. Acta. 876 (2015) 71–76. https://doi.org/10.1016/j.aca.2015.03.023
[136] X.-M. Nie, R. Huang, C.-X. Dong, L.-J. Tang, R. Gui, J.-H. Jiang, Plasmonic ELISA for the ultrasensitive detection of Treponema pallidum., Biosens. Bioelectron. 58 (2014) 314–9. https://doi.org/10.1016/j.bios.2014.03.007
[137] S.R. Ahmed, J. Kim, T. Suzuki, J. Lee, E.Y. Park, Detection of influenza virus using peroxidase-mimic of gold nanoparticles., Biotechnol. Bioeng. 113 (2016) 2298–303. https://doi.org/10.1002/bit.25982
[138] P. Luo, Y. Liu, Y. Xia, H. Xu, G. Xie, Aptamer biosensor for sensitive detection of toxin A of Clostridium difficile using gold nanoparticles synthesized by Bacillus stearothermophilus, Biosens. Bioelectron. 54 (2014) 217–221. https://doi.org/10.1016/j.bios.2013.11.013
[139] X. Ma, Y. Jiang, F. Jia, Y. Yu, J. Chen, Z. Wang, An aptamer-based electrochemical biosensor for the detection of Salmonella., J. Microbiol. Methods. 98 (2014) 94–8. https://doi.org/10.1016/j.mimet.2014.01.003
[140] Y.-C. Chang, C.-Y. Yang, R.-L. Sun, Y.-F. Cheng, W.-C. Kao, P.-C. Yang, Rapid single cell detection of Staphylococcus aureus by aptamer-conjugated gold nanoparticles, Sci. Rep. 3 (2013) 1863. https://doi.org/10.1038/srep01863
[141] B. Veigas, J.M. Jacob, M.N. Costa, D.S. Santos, M. Viveiros, J. Inácio, R. Martins, P. Barquinha, E. Fortunato, P.V. Baptista, Gold on paper–paper platform for Au-nanoprobe TB detection, Lab Chip. 12 (2012) 4802. https://doi.org/10.1039/c2lc40739f
[142] X.Z. Li, S. Kim, W. Cho, S.-Y. Lee, Optical detection of nanoparticle-enhanced human papillomavirus genotyping microarrays, Biomed. Opt. Express. 4 (2013) 187. https://doi.org/10.1364/BOE.4.000187
[143] D. Ellis, Amphotericin B: spectrum and resistance, J. Antimicrob. Chemother. 49 (2002) 7–10. https://doi.org/10.1093/jac/49.suppl_1.7
[144] B. Purkait, A. Kumar, N. Nandi, A.H. Sardar, S. Das, S. Kumar, K. Pandey, V. Ravidas, M. Kumar, T. De, D. Singh, P. Das, Mechanism of amphotericin B resistance in clinical isolates of Leishmania donovani., Antimicrob. Agents Chemother. 56 (2012) 1031–41. https://doi.org/10.1128/AAC.00030-11
[145] J.L. Italia, M.M. Yahya, D. Singh, M.N. V. Ravi Kumar, Biodegradable nanoparticles improve oral bioavailability of amphotericin b and show reduced nephrotoxicity compared to intravenous fungizone®, Pharm. Res. 26 (2009) 1324–1331. https://doi.org/10.1007/s11095-009-9841-2
[146] X. Tang, H. Zhu, L. Sun, W. Hou, S. Cai, R. Zhang, F. Liu, Enhanced antifungal effects of amphotericin B-TPGS-b-(PCL-ran-PGA) nanoparticles in vitro and in vivo., Int. J. Nanomedicine. 9 (2014) 5403–13. https://doi.org/10.2147/IJN.S71623
[147] A.M. Abraham, A. Walubo, The effect of surface charge on the disposition of liposome-encapsulated gentamicin to the rat liver, brain, lungs and kidneys after intraperitoneal administration, Int. J. Antimicrob. Agents. 25 (2005) 392–397. https://doi.org/10.1016/j.ijantimicag.2005.01.018
[148] R. Schiffelers, G. Storm, I. Bakker-Woudenberg, Liposome-encapsulated aminoglycosides in pre-clinical and clinical studies, J. Antimicrob. Chemother. 48 (2001) 333–344. https://doi.org/10.1093/jac/48.3.333
[149] M. Bala, V. Singh, A. Bhargava, M. Kakran, N.C. Joshi, R. Bhatnagar, Gentamicin Susceptibility among a Sample of Multidrug-Resistant Neisseria gonorrhoeae Isolates in India., Antimicrob. Agents Chemother. 60 (2016) 7518–7521. https://doi.org/10.1128/AAC.01907-16
[150] C. Scott, D.J. Abdelghany, R.J. Quinn, B.F. Ingram, R.F. Gilmore, C.C. Donnelly, C.J. Taggart, Gentamicin-loaded nanoparticles show improved antimicrobial effects towards Pseudomonas aeruginosa infection, Int. J. Nanomedicine. 7 (2012) 4053. https://doi.org/10.2147/IJN.S34341
[151] U. Posadowska, M. Brzychczy-Włoch, A. Drożdż, M. Krok-Borkowicz, M. Włodarczyk-Biegun, P. Dobrzyński, W. Chrzanowski, E. Pamuła, Injectable hybrid delivery system composed of gellan gum, nanoparticles and gentamicin for the localized treatment of bone infections, Expert Opin. Drug Deliv. 13 (2016) 613–620. https://doi.org/10.1517/17425247.2016.1146673
[152] S. Xie, Y. Tao, Y. Pan, W. Qu, G. Cheng, L. Huang, D. Chen, X. Wang, Z. Liu, Z. Yuan, Biodegradable nanoparticles for intracellular delivery of antimicrobial agents, J. Control. Release. 187 (2014) 101–117. https://doi.org/10.1016/j.jconrel.2014.05.034
[153] E. Yazar, A.L. Bas, Y.O. Birdane, K. Yapar, M. Elmas, B. Tras, Determination of intracellular (neutrophil and monocyte) concentrations of free and liposome encapsulated ampicillin in sheep, Vet. Med. (Praha). (2006). https://doi.org/10.17221/5517-VETMED
[154] N.M. Zaki, M.M. Hafez, Enhanced antibacterial effect of ceftriaxone sodium-loaded chitosan nanoparticles against intracellular Salmonella typhimurium, AAPS PharmSciTech. 13 (2012) 411–421. https://doi.org/10.1208/s12249-012-9758-7
[155] M.N. Seleem, N. Jain, N. Pothayee, A. Ranjan, J.S. Riffle, N. Sriranganathan, Targeting Brucella melitensis with polymeric nanoparticles containing streptomycin and doxycycline, FEMS Microbiol. Lett. 294 (2009) 24–31. https://doi.org/10.1111/j.1574-6968.2009.01530.x
[156] H. Pinto-Alphandary, A. Andremont, P. Couvreur, Targeted delivery of antibiotics using liposomes and nanoparticles: research and applications., Int. J. Antimicrob. Agents. 13 (2000) 155–68. https://www.ncbi.nlm.nih.gov/pubmed/10724019 (accessed January 2, 2019)
[157] S. Chono, T. Tanino, T. Seki, K. Morimoto, Efficient drug delivery to alveolar macrophages and lung epithelial lining fluid following pulmonary administration of liposomal ciprofloxacin in rats with pneumonia and estimation of its antibacterial effects, Drug Dev. Ind. Pharm. 34 (2008) 1090–1096. https://doi.org/10.1080/03639040801958421
[158] N. Mor, J. Vanderkolk, N. Mezo, L. Heifets, Effects of clarithromycin and rifabutin alone and in combination on intracellular and extracellular replication of Mycobacterium avium., Antimicrob. Agents Chemother. 38 (1994) 2738–42. https://www.ncbi.nlm.nih.gov/pubmed/7695255 (accessed January 2, 2019)
[159] B. Garnaik, P.N. Chaudhari, K.K. Mohite, B.S. Selukar, S.S. Nande, S.P. Parwe, Synthesis of ciprofloxacin-conjugated poly (L-lactic acid) polymer for nanofiber fabrication and antibacterial evaluation, Int. J. Nanomedicine. 9 (2014) 1463. https://doi.org/10.2147/IJN.S54971
[160] S.A. Plotkin, Vaccines: past, present and future, Nat. Med. 10 (2005) S5–S11. https://doi.org/10.1038/nm1209
[161] R.N. Germain, Vaccines and the future of human immunology, Immunity. 33 (2010) 441–450. https://doi.org/10.1016/J.IMMUNI.2010.09.014
[162] D.J. Irvine, M.C. Hanson, K. Rakhra, T. Tokatlian, Synthetic nanoparticles for vaccines and immunotherapy, Chem. Rev. 115 (2015) 11109–11146. https://doi.org/10.1021/acs.chemrev.5b00109
[163] A. Salvador, M. Igartua, R.M. Hernández, J.L. Pedraz, An overview on the field of micro- and nanotechnologies for synthetic peptide-based vaccines, J. Drug Deliv. 2011 (2011) 1–18. https://doi.org/10.1155/2011/181646
[164] S.M. Moghimi, A.C. Hunter, J.C. Murray, Nanomedicine: current status and future prospects, FASEB J. 19 (2005) 311–330. https://doi.org/10.1096/fj.04-2747rev
[165] A.S. Fauci, D.M. Morens, The perpetual challenge of infectious diseases, N. Engl. J. Med. 366 (2012) 454–461. https://doi.org/10.1056/NEJMra1108296